Does the word “pharmacology” or “medications” give you anxiety? If so, you are in good company! To help reduce some of the stress you may be feeling about the exam, let’s talk about the 50 most common medications for the NCLEX and how to tweak your exam prep to feel confident answering any pharmacology question.
Let’s get started!
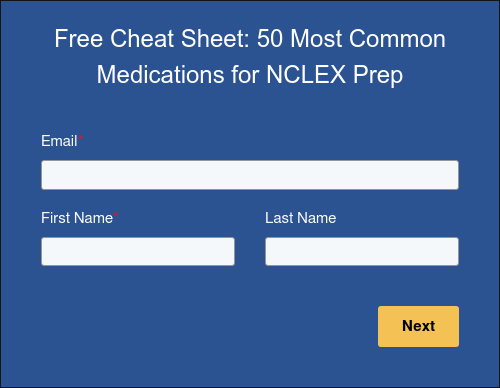
📘 FREE Download: 50 Most Common Medications for NCLEX Prep
Too long, didn’t read? Fill out the form and get the cheat sheet sent right to your inbox for FREE!
(And before you ask…yes, it’s color coded 🤩)
What are the 50 most common medications for the NCLEX?
Organized by medication type, these are the ones you really need to know:
Antihypertensives
1. Amlodipine
Use: Hypertension (HTN)
Class: Calcium channel blocker
Key fact: Watch for peripheral edema
2. Furosemide
Use: Edema, HTN
Class: Loop diuretic
Key fact: Monitor potassium, risk of ototoxicity at high doses
3. Lisinopril
Use: HTN, heart failure (HF)
Class: Angiotensin-converting enzyme (ACE) inhibitor (-pril)
Key fact: Watch for cough, angioedema, hyperkalemia
4. Losartan
Use: HTN, HF
Class: Angiotensin II receptor blocker (ARB) (-sartan)
Key fact: Similar to ACE inhibitors but no dry cough
5. Metoprolol
Use: HTN, HF, angina
Class: Beta-blocker (-olol/-ilol)
Key fact: Hold if heart rate (HR) < 60 bpm
Cardiovascular Medications
6. Adenosine
Use: Treat supraventricular tachycardia (SVT)
Class: Antiarrhythmic
Key fact: Causes brief asystole to reset rhythm – MONITOR WITH TELEMETRY!
7. Amiodarone
Use: for ventricular dysrhythmias
Class: Antiarrhythmic
Key fact: Watch for pulmonary/liver toxicity
8. Atorvastatin
Use: High cholesterol
Class: Statin
Key fact: Monitor liver function tests; watch for muscle pain (rhabdomyolysis)
9. Digoxin
Use: HF, atrial fibrillation (Afib), HF
Class: Cardiac glycoside
Key fact: Monitor for toxicity (nausea, vomiting, vision changes); check apical pulse before giving (hold if HR < 60 bpm)
10. Nitroglycerin
Use: Angina
Class: Nitrate
Key fact: Causes headache, hypotension
Anticoagulants
11. Clopidogrel
Use: Prevent clots
Class: Antiplatelet
Key fact: Increases bleeding risk
12. Enoxaparin
Use: Deep vein thrombosis (DVT), pulmonary embolism (PE)
Class: Low molecular weight heparin
Key fact: No partial thromboplastin time (PTT) monitoring
13. Heparin
Use: DVT, PE
Class: Anticoagulant
Key fact: Monitor PTT, antidote is protamine sulfate
14. Warfarin
Use: DVT, PE
Class: Anticoagulant
Key fact: Monitor international normalized ratio (INR), avoid vitamin K-rich foods
Antidiabetic Medications
15. Insulin
Use: Diabetes mellitus (DM) 1 & 2
Key fact: Lispro (rapid), regular (IV for DKA), NPH (intermediate), glargine (no peak); watch for hypoglycemia
16. Glipizide
Use: DM II
Class: Sulfonylurea
Key fact: Risk of hypoglycemia, take with food, assess allergy to sulfa drugs
17. Metformin
Use: DM II
Class: Biguanide
Key fact: Does not cause hypoglycemia; risk of lactic acidosis
Respiratory Medications
18. Albuterol
Use: Acute asthma or COPD exacerbation
Class: Short-acting beta agonist (SABA)
Key fact: Watch for tachycardia
19. Fluticasone
Use: Manage allergies or asthma
Class: Corticosteroid
Key fact: Rinse mouth after inhaler use
20. Ipratropium
Use: COPD or asthma
Class: Anticholinergic
Key fact: Commonly causes dry mouth
21. Montelukast
Use: Asthma or allergy prevention
Class: Leukotriene receptor antagonist
Key fact: Take at night
22. Salmeterol
Use: Long-term asthma or COPD management
Class: Long-acting beta agonist (LABA)
Key fact: Not for acute respiratory exacerbations
Pain Management
23. Acetaminophen
Use: Mild to severe pain, fever
Class: Analgesic, Antipyretic
Key fact: Max 4g/day; antidote is acetylcysteine; caution with liver/kidney impairment
24. Ibuprofen
Use: Mild to severe pain
Class: Nonsteroidal antiinflammatory (NSAID)
Key fact: Take with food to prevent GI upset; caution with bleed risk
25. Morphine
Use: Severe pain
Class: Opioid
Key fact: Monitor level of consciousness (LOC), watch for respiratory depression, antidote is naloxone
26. Oxycodone
Use: Moderate to severe pain
Class: Opioid
Key fact: Monitor LOC, watch for respiratory depression, not intended for long-term use
GI Medications
27. Docusate sodium
Use: Constipation
Class: Stool softener
Key fact: Promotes bowel movements
28. Pantoprazole
Use: GERD
Class: Proton pump inhibitor (PPI) (-azole)
Key fact: Take before first meal of day; long-term use increases risk for fractures
Neuro/Mental Health Medications
29. Alprazolam
Use: Anxiety and panic disorders
Class: Benzodiazepine
Key fact: Risk of dependence, do not stop taking suddenly
30. Donepezil
Use: Mild to moderate dementia (Alzheimer disease)
Class: Acetylcholinesterase inhibitor
Key fact: Take at bedtime, may cause GI upset
31. Fluoxetine
Use: Depression, anxiety disorder
Class: Selective serotonin reuptake inhibitor (SSRI)
Key fact: Monitor for serotonin syndrome (fever, confusion); 4-6 weeks to take effect
32. Gabapentin
Use: Seizure prophylaxis or neuropathic pain
Class: Anticonvulsant
Key fact: Taper off slowly; avoid alcohol
33. Haloperidol
Use: Acute psychosis, schizophrenia
Class: Neuroleptic (nonphenothiazine)
Key fact: Watch for extrapyramidal symptoms (EPS), QT prolongation, neuroleptic malignant syndrome (NMS)
34. Lithium
Use: Bipolar disorder (mania), schizophrenia
Class: Mood stabilizer
Key fact: Narrow therapeutic range (0.6–1.2), avoid dehydration
35. Olanzapine
Use: Schizophrenia, bipolar disorder, depression
Class: Atypical antipsychotic
Key fact: Watch for weight gain, metabolic syndrome
36. Memantine
Use: Moderate to severe dementia (Alzheimer disease)
Class: NMDA receptor antagonist
Key fact: May cause dizziness or rash
37. Phenytoin
Use: Seizures
Class: Anticonvulsant (hydantoin)
Key fact: Monitor therapeutic range (10-20 mcg/mL); watch for gingival hyperplasia
38. Zolpidem
Use: Insomnia
Class: Sedative-hypnotic (nonbenzodiazepine)
Key fact: Meant for short-term use; avoid other CNS depressants
Antibiotics/Antivirals
39. Amoxicillin
Use: Respiratory infections, urinary tract infections, etc.
Class: Broad-spectrum penicillin
Key fact: Watch for allergy, take full antibiotic course
40. Azithromycin
Use: Upper and lower respiratory, sexually transmitted, and skin infections
Class: Macrolide
Key fact: QT prolongation, take on an empty stomach
41. Ciprofloxacin
Use: Respiratory, urinary, skin, eye, and ear infections
Class: Fluoroquinolone
Key fact: Risk of tendon rupture; avoid in pediatrics
42. Gentamicin
Use: Serious infections including sepsis, MRSA, and endocarditis
Class: Aminoglycoside
Key fact: Watch for ototoxicity and nephrotoxicity
43. Metronidazole
Use: Anaerobic bacterial infections, Clostridioides difficile infection, acne rosacea
Class: Nitroimidizole
Key fact: NO alcohol; causes disulfiram-like reaction
44. Vancomycin
Use: Serious infections like endocarditis, MRSA, Clostridioides difficile, and respiratory/skin/bone infections
Class: Glycopeptide
Key fact: Monitor for vancomycin flushing syndrome (red man syndrome); monitor trough levels
OB
45. Methylergonovine
Use: Prevention and treatment of postpartum hemorrhage
Class: Uterotonic
Key fact: Avoid with hypertension
46. Oxytocin
Use: Labor induction or prevention and treatment of postpartum bleeding
Class: Uterotonic (oxytocic agent)
Key fact: Monitor for uterine hyperstimulation, fetal intolerance
Other Need-to-know Medications
47. Levothyroxine
Use: Hypothyroidism
Class: Thyroid hormone
Key fact: Take on an empty stomach in the morning
48. Epoetin alfa
Use: Anemia
Class: Biologic response modifier
Key fact: Stimulates RBCs; monitor Hgb; risk of hypertension
49. Potassium chloride
Use: Hypokalemia
Class: Electrolyte replacement
Key fact: NEVER push IV; dilute to avoid phlebitis; monitor potassium levels and cardiac rhythm
50. Methotrexate
Use: RA, cancer
Class: Folic acid antagonist
Key fact: Avoid in pregnancy; monitor bone marrow suppression, liver function
How do you memorize the most common NCLEX medications to study?
1. Break down the material into digestible chunks.
It can be overwhelming to think about reviewing everything you learned in pharmacology, right? If you’re feeling this way, try breaking these 50 most common medications for NCLEX prep into manageable chunks. Group and prioritize the material in a way that makes sense to you.
Here are some examples:
Focus on medication classes.
Learn your mechanisms of action, common side effects, and any pertinent safety information.
Don’t dive into every individual medication in a drug class. Instead, focus on key examples within the drug class.
Example: Use metoprolol for beta blockers.
Group medications by system.
Study medications and medication classes by the body system that they’re intended to be used for.
Example: The cardiovascular system involves beta blockers, ACE inhibitors, calcium channel blockers, etc.
Prioritize “must know” medications.
The NCLEX will test your knowledge and understanding of drugs that are common in practice or present possible safety issues.
If you need help figuring that list out, go back up to our list of the 50 most common medications and take a screenshot (or even print it out) for easy reference!
2. Use memory tools.
Use memory tools, mnemonics, songs, acronyms—whatever works for you! Memory tools can help solidify key concepts of pharmacology in your mind (I always found the sillier the memory tool, the better!).
For example, use “SPironoloactone – Spares Potassium” to remember that spironolactone is a potassium sparing diuretic! The goal is to make learning the 50 most common medications for the NCLEX, or any nursing subject, fun and memorable!
3. Use active recall!
Active recall is a study method where you actively retrieve information from memory, rather than passively reviewing it. A great tool for this is the Feynman technique:
Here’s how it works: Take what you’re studying and put complex ideas into simple terms. For example, pretend you’re teaching a patient about a new medication. Finding a way to talk about the medication in your own words forces you to truly understand the material, not just memorize it.
Engaging with the material this way helps strengthen your knowledge and makes it easier to recall at another time…like during the NCLEX!
4. Find a Qbank to practice answering NCLEX-style questions.
This is a tip that we cannot stress enough! Personally, I split my study time between active recall study sessions and using a Qbank for NCLEX practice questions. Including NCLEX practice question sessions in your studying will help you practice recalling information and get you into the real deal RN mindset!
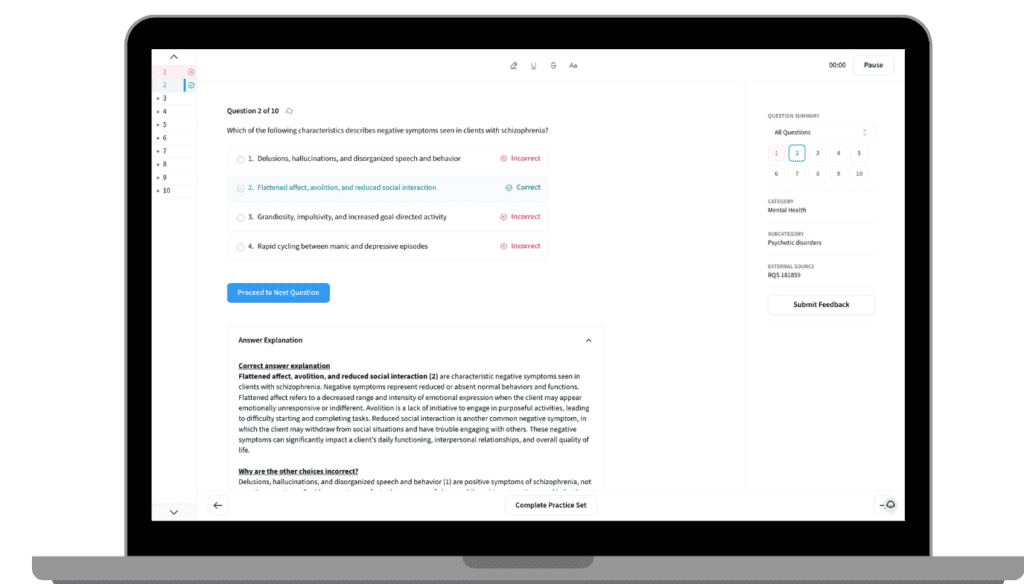
Speaking of Qbanks, check out Blueprint’s NCLEX Qbank with 1,000+ practice questions based on the NCSBN NCLEX Test plan!
Want a sneak peek of the Qbank? Here’s one of our pharmacology questions straight from the Qbank:
Practice Question
The nurse in the labor and delivery unit is monitoring a client who is receiving intravenous (IV) oxytocin. The client demonstrates an adequate contraction pattern with contractions every 2–3 minutes, lasting 50–60 seconds. Which of the following actions should the nurse take?
A) Decrease the infusion rate per the provider’s order.
B) Discontinue the infusion per the provider’s order.
C) Document and continue to monitor.
D) Increase the infusion rate per the provider’s order.
Correct Answer: C
Oxytocin is a synthetic hormone that stimulates the smooth muscle contraction of the uterus during labor induction. It can be used to strengthen uterine contractions during labor, control postpartum hemorrhage, and decrease uterine atony. The rate of infusion of oxytocin given during labor should be titrated based on uterine and fetal response. Once labor has begun, the goal of oxytocin administration is to promote an adequate contraction pattern that progresses labor with contractions every 2–3 minutes that last 50–60 seconds. Since the client has met this goal, the nurse should document the findings and continue to monitor them (3). Maternal vital signs, fetal heart rate, and contractions should be monitored closely to adjust the infusion as needed.
Why are the other choices incorrect?
The client is exhibiting an adequate contraction pattern, and it is not necessary to decrease the infusion rate (1). However, if the client develops tachysystole, more than five contractions within 10 minutes for two consecutive 10-minute periods, then it would be appropriate for the nurse to decrease the infusion rate per the provider’s order. As long as the client and the fetus are hemodynamically stable, there is no indication for the nurse to discontinue the infusion (2). If there is fetal distress or signs of intolerance, the infusion may be discontinued after notifying the provider. Increasing the infusion rate (4) could increase the risk of tachysystole and complications such as fetal distress or uterine rupture. Excessive and frequent contractions reduce blood flow to the uterus and placenta and can stretch the uterine muscle, making it prone to tearing. The nurse should monitor the client for increased pain, loss of contractions, and fetal heart rate decelerations.
Where are some other places to get practice?
Need to find resources to help get you going? Check out some of our study essentials:
👩💻 NCLEX Live Study Group
📚 NCLEX Self-Paced Crash Course
📈 NCLEX Qbank (Sign up for a FREE sneak peek!)
🍎 FREE NCLEX Prep Classes
📱Our TikTok (Check out Abby’s medication Mondays!)
Final Thoughts
Alright, those are the 50 most common medications for NCLEX prep and how to study like a pharmacology pro! Remember, it’s not all about memorizing every detail for every medication! It’s about knowing how to focus on your med class basics, some specific key facts, and safety considerations that would impact your client on the NCLEX and in real life.
Just be consistent with your studying and let us be your study buddy along the way. Now, go crush it!
Looking for even more (free!) content to help you crush the NCLEX? Check out these other cheat sheets: