Studying for the NCLEX and feeling overwhelmed by medication questions? You’re not alone! Metronidazole (also known by its brand name Flagyl) is one of those medications that loves to show up on the NCLEX, and for good reason—it’s commonly prescribed and has some pretty important nursing considerations you absolutely need to know.
Let’s break down everything you need to understand about metronidazole nursing considerations so you can tackle those NCLEX questions with confidence. We’ll cover the must-know side effects, critical contraindications, and essential client teaching points that could make or break your exam performance.
Ready to master this antibiotic? Let’s dive in!
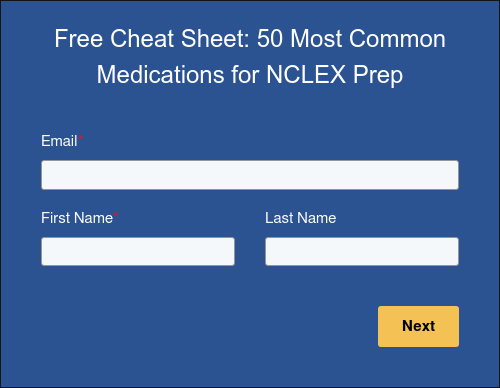
💊 Free Download: 50 Most Common Medications to Know for the NCLEX
Want to skip ahead a bit? Our team of experts put together a FREE cram sheet with the most common medications to know for the NCLEX! Just fill out the form below and get the cheat sheet directly in your inbox. 💡
What Is Metronidazole and How Does It Work?
Metronidazole is an antibiotic that specifically targets bacterial and parasitic infections. Think of it as your go-to medication for infections in the vagina (like bacterial vaginosis), stomach, liver, and trichomoniasis (a sexually transmitted infection caused by parasites).
Here’s the cool part about how it works: metronidazole actually enters the bacterial cell and binds directly to the bacteria’s DNA. This binding process leads to the death of the bacteria, effectively clearing up the infection.
This medication is particularly effective against anaerobic bacteria (bacteria that don’t need oxygen to survive) and certain parasites, which is why it’s such a valuable tool in treating specific types of infections.
Common Side Effects Every Nurse Should Know
When it comes to metronidazole nursing considerations, understanding side effects is crucial for both client safety and NCLEX success. The most common side effects revolve around gastrointestinal issues, so let’s talk about what your clients might experience.
Gastrointestinal Upset
GI upset is hands-down the most frequent complaint with metronidazole. Your clients might experience:
- Nausea and vomiting
- Diarrhea
- Decreased appetite
- General stomach discomfort
This is exactly why client teaching about taking metronidazole with food is so important—it can significantly reduce these uncomfortable GI side effects.
The Infamous Metallic Taste
Here’s a side effect that clients often find particularly bothersome: a metallic taste in their mouth. This isn’t dangerous, but it can be really unpleasant and may affect their appetite or enjoyment of food. Let your clients know this is normal and temporary—it’ll resolve once they finish their course of medication.
Severe Side Effects That Require Immediate Attention
While most clients tolerate metronidazole well, there are some serious side effects that require immediate nursing intervention and client education.
Peripheral Neuropathy
Though rare, peripheral neuropathy can occur with metronidazole use, especially with prolonged treatment. Watch for signs like:
- Tingling or numbness in hands and feet
- Muscle weakness
- Pain or burning sensations in extremities
If clients report any of these symptoms, they need to contact their healthcare provider immediately.
Seizures
Seizures are another rare but serious side effect. Clients with a history of seizures or CNS disorders may be at higher risk. This is why taking a thorough medical history is so important before administering metronidazole.
Critical Contraindications: The Big No-Nos
This is where metronidazole nursing considerations get really important for client safety. There are several substances and situations where metronidazole should absolutely be avoided.
Alcohol and Disulfiram Interaction
Here’s the big one that NCLEX loves to test: clients must avoid alcohol completely while taking metronidazole and for at least 24-48 hours after their last dose. This includes:
- Alcoholic beverages
- Medications containing alcohol
- Mouthwash with alcohol
- Cooking wines or extracts
The combination can cause a disulfiram-like reaction with symptoms including severe nausea, vomiting, flushing, headache, and rapid heart rate. Clients should also avoid disulfiram (Antabuse) itself.
Propylene Glycol Warning
Foods and medications containing propylene glycol should also be avoided, as they can cause similar adverse reactions when combined with metronidazole.
Breastfeeding Considerations
If a breastfeeding parent needs metronidazole, they should avoid breastfeeding for 24 hours after taking each dose. The medication passes into breast milk and could potentially harm the nursing infant.
Essential Administration Instructions
Getting the administration right is crucial for both medication effectiveness and client comfort.
Extended-Release Tablets: Handle with Care
If your client is prescribed extended-release metronidazole tablets, they must swallow them whole. No crushing, chewing, or breaking these tablets! This could lead to too much medication being released at once, increasing the risk of side effects.
Food Timing Matters
Always instruct clients to take metronidazole with food. This simple step can significantly reduce those uncomfortable GI side effects we talked about earlier. It’s such a straightforward intervention that can make a huge difference in client comfort and medication adherence.
Key Metronidazole Nursing Considerations
As a nurse, your role extends far beyond just administering the medication. Here are the essential nursing considerations that will serve you well on the NCLEX and in clinical practice.
Client Education Is Everything
Your teaching should cover:
- The importance of completing the full course of antibiotics, even if symptoms improve
- Alcohol avoidance (cannot stress this enough!)
- Taking medication with food to reduce GI upset
- Reporting any signs of neurological changes immediately
- Breastfeeding precautions if applicable
Monitoring and Assessment
Keep an eye out for:
- GI side effects and client tolerance
- Signs of peripheral neuropathy (tingling, numbness, weakness)
- Any neurological changes, including seizure activity
- Client adherence to alcohol restrictions
Documentation Points
Document:
- Client’s understanding of medication instructions
- Any side effects experienced
- Compliance with alcohol restrictions
- Response to treatment
Test Your Knowledge with a Practice Question!
Ready to put all this knowledge into action? Check out this NCLEX practice question on metronidazole:
Your Path to NCLEX Success
Understanding metronidazole nursing considerations isn’t just about memorizing facts—it’s about putting client safety first and demonstrating critical thinking skills that the NCLEX is designed to test.
Remember these key takeaways: metronidazole is an effective antibiotic for bacterial and parasitic infections, but it requires careful client education about alcohol avoidance, proper administration with food, and monitoring for serious side effects like peripheral neuropathy.
The most important thing? Always prioritize client safety by ensuring they understand the critical importance of avoiding alcohol while taking this medication. This knowledge will serve you well on exam day and throughout your nursing career.
Ready to tackle more NCLEX questions? Get 60 days of FREE access to Blueprint’s Complete Self-Prep Package, including 23 hours of video lessons, 17 quizzes, 2,000+ practice questions, a predictor exam, and more!
And for more (free!) NCLEX content, check out these other posts on the blog: