Return to Blog
Homepage
The Challenge of Constructive Feedback in Medical Education
- by
- Apr 26, 2022
- Reviewed by: Amy Rontal, MD
There are few things more unbearable than mandatory meetings about burnout. It usually goes something like this: the institution tells you why you are burnt out, then offers a paradoxical solution to the problem.
You are burned out because you are not getting enough sleep. On Thursday morning, we need you to come in an hour earlier than expected, so that you can get lectured to, for an hour, on the importance of sleep. Sacrifice some sleep so that you can learn why you should get more sleep.
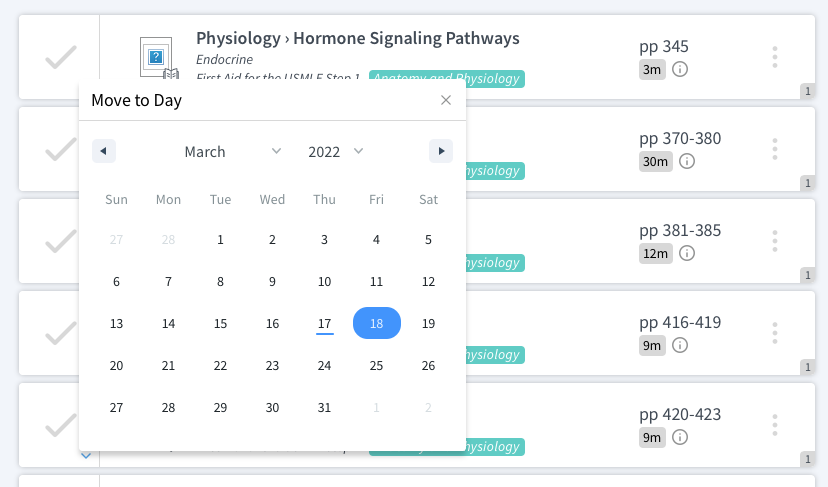
Another one I encountered in training: You are getting burned out because you are working too much and not receiving feedback regarding your work. We’ve created a feedback program which will entail both attendings and residents logging onto an esoteric system and completing daily feedback forms. Here’s some extra work to treat your burnout.
While the implantation was a little off, feedback is an important part of medical training. With the nature of training, it is essential for trainees to know how to get better at everything they do. And naturally, the need to deliver feedback gracefully must become part of your skill set at some point.
As I moved onto the attending role, the challenge of giving feedback stuck with me. Sometimes it was an easy directive, like “Don’t put your face 4 inches from the patient’s mouth while intubating. Stand up tall.” Simply deliver the finer points of technique to help the student or resident excel.
Other feedback takes a little more tact in delivery. As an attending anesthesiologist, I am often typing up pre-ops while monitoring the status of my 3 rooms on the EMR, just to get a sense of how things are going. Some residents/CRNAs use the phrase “stalking the chart.” The importance of word choice is paramount here. I could convey a message that says “I don’t trust you, so I’m keeping a close eye on things in the background.” But in reality, I do trust them, but I have an equal concern for the well-being of the patient, and having both our sets of eyes on vitals is certainly a safer option than just one set. “S/he’s my patient, too,” I tell them with a smile.
During a recent chart check, I noticed that in one of our tenuous patients with pre-existing biventricular failure, no blood pressure had been checked in 20 minutes. This created a frightening scenario, and I immediately jogged up to the room.
I was left asking, “What do I say to rectify this problem, improve the practice of my resident, and not sound like a jerk?” Accomplishing all 3 is a tricky endeavor.
“Steve, you haven’t checked a blood pressure in 20 minutes. This is a breach in the standard of care.” I said this sternly while keeping a level head, and cycling the cuff myself. So why did I choose to say it in this way?
I stated objective facts. There was no judgement on the habits of acumen of the resident. No blaming or curses or raised voice. Clearly he knows he made a mistake and dropped the ball in attentiveness. While I was most disappointed in the disregard for the patient’s safety, “reaming out” the offender wouldn’t have done anyone any favors. I went on, “You have about 5 core things to monitor, you have to pay attention to all of them. It’s definitely within your capabilities.” In not so many words, I told Steve that he is better than this level of care.
After further investigation, I learned there was a switch from a portable monitor to the stationary monitor, and automatic blood pressure wasn’t resumed. It was an honest mistake, but one that certainly should have been noticed and rectified earlier.
Later in the day, I find another resident providing a bedside TEE in the ICU. The patient suffered a cardiac arrest and was found to also have a very sick heart, and further investigation with TEE was necessary. The patient was morbidly obese, which would make sedating him for this case an even greater challenge. But this resident is someone I know I can trust to do the right thing.
I arrive to the room midway through the case to find that this case is being performed without an end-tidal CO2 monitor, one of the necessary monitors for a sedation procedure, especially in a remote location like an ICU. Words come to me: “Why the hell are you doing this case without end-tidal?” But instead, a more diplomatic approach centers itself in my mind: “Carly, performing this case without end-tidal is definitely making it less safe for the patient.” We asked the ICU nurse to provide the necessary monitors, and we successfully navigated through the situation. Carly knows what she should have done; there is no need for me to be paternalistic and explain this to her.
Whether you are in a medical student, resident, or attending role, giving and receiving feedback is going to be crucial to your day-to-day practice. You will come to learn the undeniable importance of being an excellent communicator. And there can be so much that goes into the delivery of a simple message, so it is a necessity to think about exactly what you will say, and how you will say it, in order to achieve your goal and get through to your pupil. Here are some basic tenets to keep in mind to make sure you get your point across clearly and effectively.
Select the right time and place to deliver your message
Sometimes, the information must be given immediately. “Don’t hold the instrument like that, put your fourth finger through the hole.” “Your chest compressions aren’t deep enough, go harder.” Disclosing this information at a debriefing after the event wouldn’t be as effective.
However, some feedback is better given after the fact. “I think you can do a better job at task delegation during the code,” is better left to being disclosed after the code, instead of in the heat of the moment.
Also consider, would you be better off discussing this seated at a round table where notes can be reviewed and the environment is relaxed? Or will your message be more effective if given in another location?
Think about your real mission
In giving feedback, are you merely trying to check a box to say that you gave feedback? Is your goal to applaud the excellent medical student, and take the wind out of the sails of the weaker one? Certainly not. My goals in the above scenarios were a) make sure that resident A elevated their vigilance for every case for the rest of their career, and b) get resident B to use the necessary monitors for every case, especially in the out of OR settings. I wasn’t looking to put anyone down, lift anyone up, or make myself feel something. I wanted my residents to be the safest practitioners, and take the best possible care of their patients.
Refer to actions, not character traits
Naturally, you don’t want to tell someone that they have a problem. “Sally, you just don’t get it.” “Jim, procedures really aren’t your thing.” “Carl, your pace isn’t fast enough for this field.”
Rather, it is better to refer to particular decisions or actions that would be easier to change than a facet of someone character. “Sally, opting for crystalloid instead of pressor was not what the evidence suggests is a best practice.” “Jim, it took 40 minutes to place that central line. Let’s break it down and see where you might have gotten held up.” “Carl, we can’t afford to focus on the minutae of the patient’s history when there are larger priorities in their emergent care that must be addressed right now.”
Frame every mishap as a teachable moment
You’re teaching the future leaders for a reason. You have previously made the mistakes that they are making now, and it is your job to help them correct and avoid such mistakes in the future. If they executed perfectly, you’d have little to offer in terms of improvement. Try to see every instance where things didn’t go so well as an opportunity to send a message to the resident or medical student that will stick with them forever. Like Master Yoda says, “The most incredible teacher, failure is.”
Be honest in all of your deliveries, and remember your purpose: to train the up and comers to be fantastic physicians. If your actions and words and chosen with this goal in mind, you will always opt for the right course of action.
Further reading: