The Ultimate Patient Case Presentation Template for Med Students
- by
- Apr 06, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.
 Looking for some help studying your shelf/Step 2 studying with clinical rotations? Try our combined Step 2 & Shelf Exams Qbank with 5,500 practice questions—free for 7 days!
Looking for some help studying your shelf/Step 2 studying with clinical rotations? Try our combined Step 2 & Shelf Exams Qbank with 5,500 practice questions—free for 7 days!
7 Ingredients for a Patient Case Presentation Template
1. The One-Liner
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint.
I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
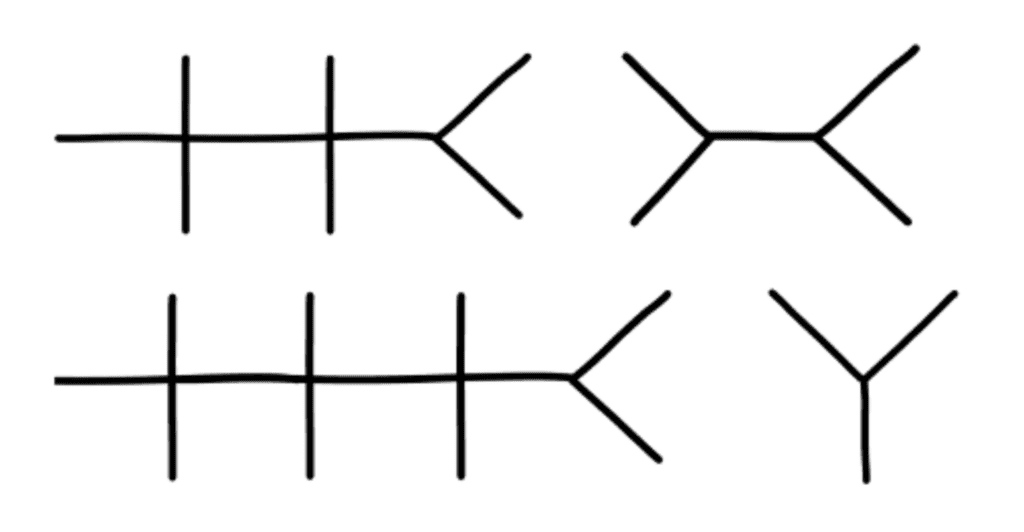
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Onset
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
Provocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Quality
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
Region/Location
Indicate where the pain is located and if it radiates anywhere.
Severity
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Timing
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting.
Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply.
In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing.
I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history.
As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview.
By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis.
Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition.
One way of organizing the social history is the HEADSSS method:
– Home living situation and relationships
– Education and employment
– Activities and hobbies
– Drug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use.
– Sexual history (partners, STI history, pregnancy plans)
– Suicidality and depression
– Spiritual and religious history
Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital Signs
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives. When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning.
For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.”
Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Labs
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section.
This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain.
Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan.
It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability.
Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another.
Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points.
You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest.
One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.
A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs.
One-Liner:
Chief Complaint:
History of Present Illness:
Past Medical History:
Past Surgical History:
Family History:
Social History:
Medications:
Allergies:
Immunizations:
ROS:
Objective:
Vital Signs: Temp ___ BP ___ /___ HR ___ RR ___ O2 sat ___
Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Pulmonary:
Breast:
Abdominal:
Genitourinary:
Musculoskeletal:
Skin:
Labs:
Most Recent Labs:
Previous Labs:
Diagnostics/Imaging:
Study:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
Plan:
#Problem 2:
Assessment:
Plan:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide.
Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history. Nonetheless, the aforementioned template should set you up for success from a broad overview perspective.
Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at neelesh.bagrodia@blueprintprep.com!
Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
About the Author