Can You Diagnose This Condition?
July
A 38-year-old woman presents to the emergency department with an eyelid laceration sustained during a bar fight. The laceration is shown above. She has normal visual acuity, no corneal abrasions noted on fluorescein staining, and normal intraocular pressures. Her extraocular muscles are intact as well. What is the appropriate next step in management?
A) Consult ophthalmology
B) Discharge with an eye patch and close follow-up
C) Repair with 6-0 sutures
D) Repair with tissue adhesive
Answer: Consult ophthalmology
The patient is presenting with an eyelid laceration with orbital fat protrusion, indicating damage to the orbital septum, which requires an emergent ophthalmology consult. The structures surrounding the eyelids are delicate, and lacerations to the eyelids should be approached carefully in the emergency department. Failure to diagnose structural injuries can lead to functional as well as cosmetic defects.
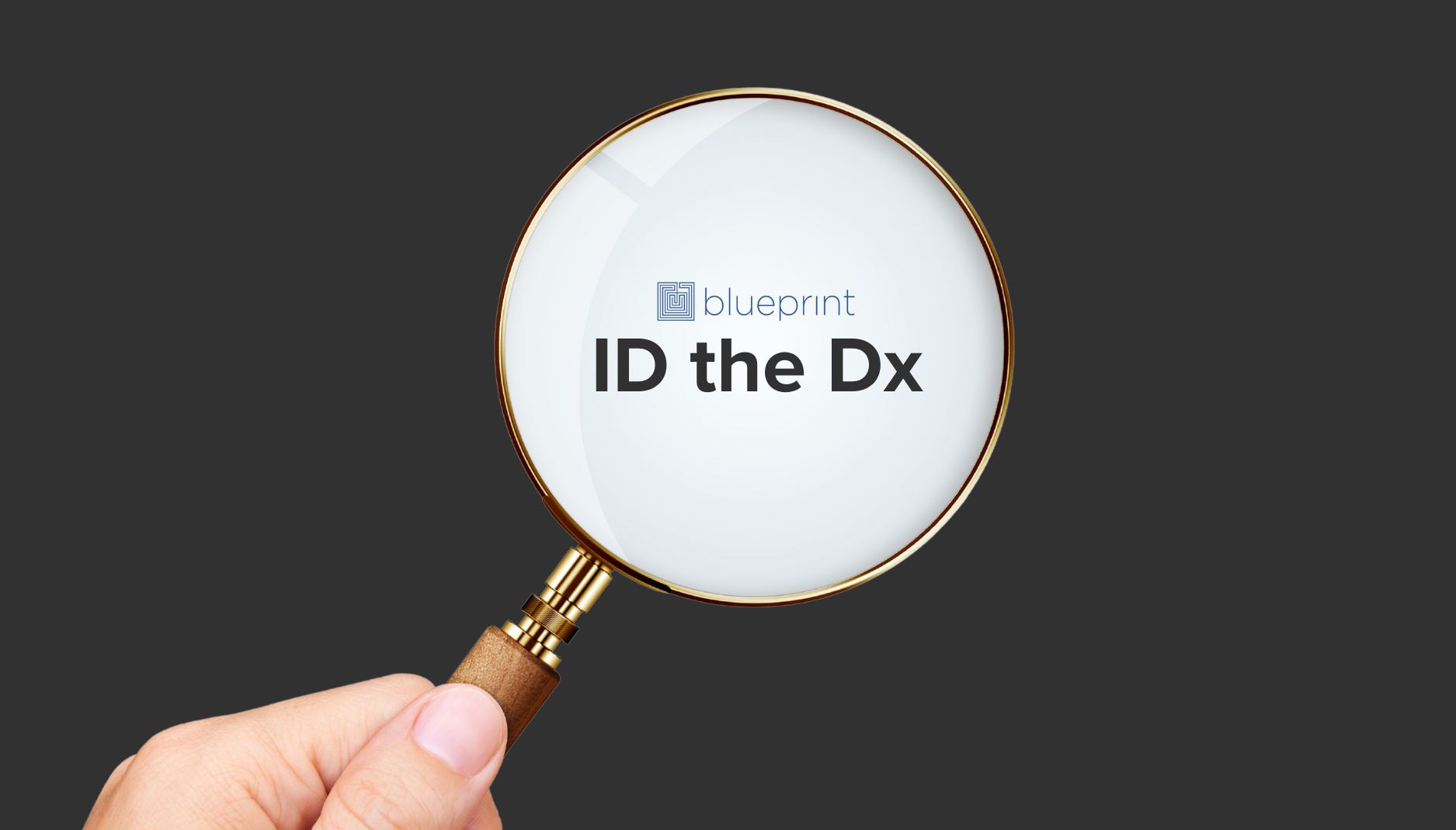
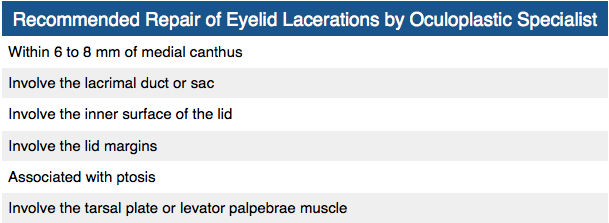
For all eyelid lacerations, the integrity of the globe and orbital structures should be examined first. Next, the eyelid should be examined to assess for involvement of the canthi, lacrimal system, and orbital septum. Lacerations that involve the lid margin, are within 6–8 mm from the medial canthus, present with ptosis, involve the inner surface of the lid, or suggest damage to the orbital septum should be repaired by an oculoplastic specialist. The orbital septum is a membranous sheet that acts as the anterior boundary of the orbit. If orbital fat is able to protrude from a laceration, it is a sign of an orbital septal defect and suggests damage to surrounding muscles of the eye, which can lead to ptosis if not repaired correctly.
Discharging a patient with an eye patch and close follow-up (B) should not be done in the emergency department without specific instructions and confirmed urgent follow-up by an oculoplastic specialist.
Repairing the laceration with sutures (C) or tissue adhesive (D) would also be inappropriate. When damage to the orbital septum is suspected, repair should be done by an oculoplastics specialist to minimize functional and cosmetic defects. If there is a superficial laceration that does not meet the criteria for specialist referral, 6-0 or 7-0 sutures can be considered for repair. Tissue adhesives should be avoided for all injuries close to the eye, as there is a high chance of corneal abrasions and bonding the eyelids together.
June
A 64-year-old woman is brought to the primary care physician by her son because of progressive memory loss over the past 9 months. Due to this memory loss, she is now unable to perform activities of daily living. Over this time period, she has had frequent episodes of diarrhea but no nausea or vomiting. She smokes half a pack of cigarettes and drinks five to six beers daily. Her temperature is 36.8°C, heart rate is 82 bpm, and blood pressure is 115/79 mm Hg. On mental status examination, she is oriented to person only. She cannot recall any objects after 5 or 10 minutes. Examination shows a hyperpigmented rash on her neck, as seen in the provided image. Which of the following deficiencies is most likely present in this patient?
A) Ascorbic acid
B) Niacin
C) Pyridoxine
D) Riboflavin
E) Thiamine
F) Zinc
Answer: Niacin
Niacin, also referred to as vitamin B3, is an essential vitamin used to synthesize nicotinamide adenine dinucleotide, which plays a key role in redox reactions. Niacin deficiency may occur due to a number of causes, including malnutrition, heavy alcohol consumption, vitamin B6 deficiency, and conditions associated with tryptophan deficiency, as niacin is derived from tryptophan. Hartnup disease and carcinoid syndrome may both result in tryptophan deficiency.
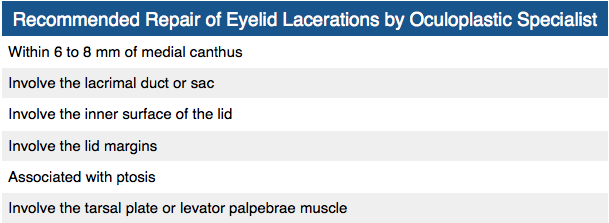
The clinical features of severe niacin deficiency, referred to as pellagra, can be recalled with the three Ds: dementia, dermatitis, and diarrhea. Specifically, the characteristic rash of pellagra is a circular collar rash on the neck and hyperpigmented lesions in areas exposed to the sun that occur due to photosensitivity. In addition to dementia, other neurologic symptoms of pellagra include hallucinations, insomnia, and anxiety.
Ascorbic acid (A), which is also called vitamin C, functions as an antioxidant and also facilitates iron absorption. It is necessary for collagen synthesis and plays a key role in the conversion of dopamine to norepinephrine. Vitamin C is commonly found in fruits and vegetables. Scurvy occurs as a result of vitamin C deficiency and is characterized by swollen gums, bruising, petechiae, hemarthrosis, anemia, and “corkscrew” hair.
Pyridoxine (C), or vitamin B6, is converted to pyridoxal phosphate, which is a cofactor used in transamination and decarboxylation reactions. It is involved in the synthesis of various neurotransmitters as well as heme, niacin, and histamine. Deficiency may occur as a result of isoniazid and oral contraceptive use. Convulsions, hyperirritability, peripheral neuropathy, and sideroblastic anemia are some of the clinical findings of pyridoxine deficiency.
Riboflavin (D), which is also called vitamin B2, is a component of the flavins, such as flavin adenine dinucleotide, which are used as cofactors in redox reactions. Riboflavin deficiency leads to cheilosis (inflammation of the lips and fissures at the mouth corners) and corneal vascularization.
Thiamine (E), or vitamin B1, functions in thiamine pyrophosphate, which is a cofactor for several key enzymatic reactions. Deficiency leads to impaired glucose breakdown. There are multiple clinical manifestations of thiamine deficiency, including Wernicke-Korsakoff syndrome, dry beriberi, and wet beriberi. Wernicke-Korsakoff syndrome is characterized by ophthalmoplegia, confusion, and ataxia. Wet beriberi consists of high-output heart failure, while dry beriberi is characterized by polyneuropathy and muscle wasting.
Zinc (F) is a mineral that is essential for the activity of many enzymes. Causes of zinc deficiency include inadequate dietary intake, acrodermatitis enteropathica, and Crohn disease. Zinc deficiency is characterized by immune dysfunction, impaired wound healing, hypogonadism, diarrhea, alopecia, and perioral dermatitis.
May
Image Source: Rosh Review
A 25-year-old woman presents to your office because she noticed a nonpainful oral ulcer as shown in the photo above. The patient reports having unprotected vaginal and oral sex with multiple partners during the last 3 months. Based on your suspected diagnosis, which of the following diagnostic tests, if positive, will provide a presumptive diagnosis of the disease?
A) Herpes simplex virus type 1 antibody
B) Rapid plasma reagin and chemiluminescence immunoassay
C) Rapid plasma reagin and VDRL
D) Tzanck smear
Answer: Rapid plasma reagin and chemiluminescence immunoassay
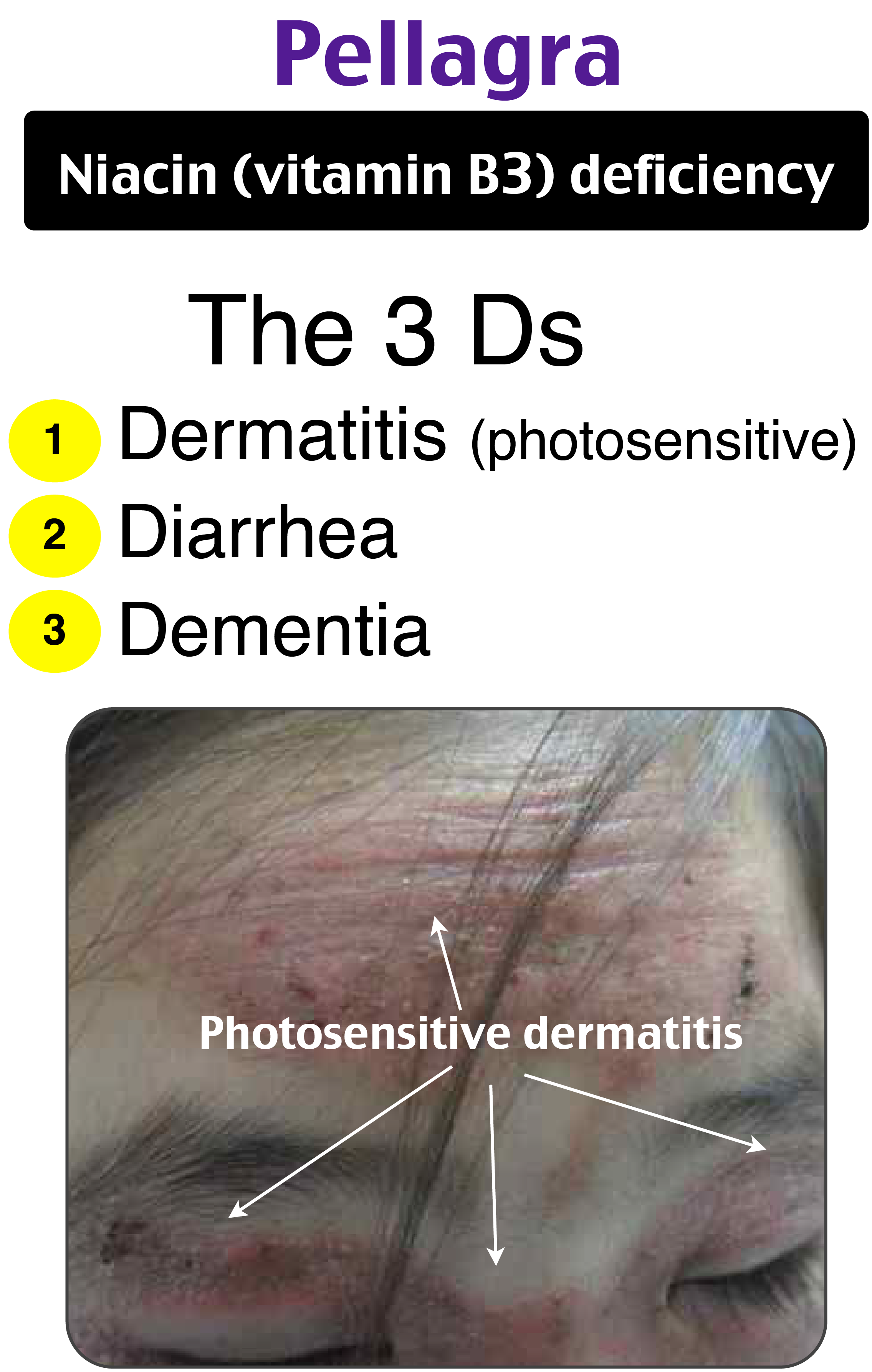
Syphilis is a disease caused by Treponema pallidum. Primary syphilis usually presents as a single painless ulcer or chancre at the site of infection, as shown in the photo above, but it may also present with multiple, painful lesions. A presumptive diagnosis of syphilis requires the use of two serologic tests: a nontreponemal test and a treponemal test. Nontreponemal tests are based on the reactivity of the patient’s serum to a cardiolipin-cholesterol-lecithin antigen. These tests include the rapid plasma reagin (RPR), VDRL, and toluidine red unheated serum test. The treponemal tests are based on the detection of antibodies against specific treponemal antigens. These tests include the fluorescent treponemal antibody absorption, microhemagglutination test for antibodies to Treponema pallidum, Treponema pallidum particle agglutination assay, Treponema pallidum enzyme immunoassay, and chemiluminescence immunoassay. The traditional algorithm follows the rule that a nontreponemal test is contacted first, and if it is reactive, infection is confirmed with a treponemal test. The most frequently nontreponemal tests used are VDRL and rapid plasma reagin, and chemiluminescence immunoassay and Treponema pallidum enzyme immunoassay are the most frequent treponemal.
Rapid plasma reagin and VDRL (C) are both nontreponemal tests and cannot be the only tests used for presumptive diagnosis of syphilis. Primary herpes simplex virus (HSV) infection typically presents with multiple vesicles, which may coalesce into a painful shallow ulcer and with local lymphadenopathy. Systemic symptoms may be present. In adults, it may also present as severe pharyngitis. Recurrent herpes simplex virus typically presents as localized ulceration at the vermilion border, but it may also appear on the buccal intraoral surface. Presumptive diagnosis is made by positive Tzanck smear (D) of the lesion. This test has poor sensitivity and specificity. There is a limited role for serology testing for diagnosis of herpes simplex virus, as primary infection may be diagnosed in patients who are HSV antibody negative and many available assays for HSV are inaccurate. Furthermore, herpes simplex virus type 1 antibody (A) can verify the type of HSV (HSV-1 or HSV-2 ) but not the location of infection (i.e., oral or genital HSV-1).
April
Image Source: Rosh Review
A 23-year-old man presents after a fight. His eye is seen above. Physical examination reveals intact extraocular movements, normal fluorescein staining, normal intraocular pressure, and normal visual acuity. What management is indicated?
A) Healing by secondary intention
B) Laceration repair by the emergency physician
C) Ophthalmology consultation for repair
D) Tissue adhesive for repair
Answer: Ophthalmology consultation for repair
This patient presents with a complex eyelid laceration possibly involving the canalicular system and should have a consultation with either ophthalmology or plastic surgery regarding repair. It is important to search for a penetrating globe injury in any patient with an eyelid laceration because of the proximity of structures. Simple horizontal and partial thickness lid lacerations can be repaired primarily by an emergency physician. However, more complicated lacerations should be considered for specialist repair because of the high likelihood of cosmetic or functional complications, or both. In general, lacerations through the orbital septum, lacerations with tissue loss, lacerations involving the lid margins, lacerations involving the levator or canthal tendons, and those involving the canalicular system should be repaired by a skilled ophthalmologist or plastic surgeon. Injury to the canalicular system should be suspected in any laceration involving the medial lower eyelid.
Tissue adhesive (D) is contraindicated this close to the eye and should not be used in an injury that requires precision alignment of tissue. Healing by secondary intention (A) will likely lead to worse cosmetic outcomes and is inappropriate when the canalicular system is involved. Primary repair by the emergency physician (B) is not recommended if the canalicular system may be involved.
March
Image Source: Rosh Review
A 66-year-old man presents to the emergency department with a facial droop. His symptoms started last night and have worsened since then. His temperature is 99.0°F (37.2°C), blood pressure is 135/84 mm Hg, pulse is 76/min, respirations are 19/min, and oxygen saturation is 99% on room air. Physical exam reveals a right-sided facial paralysis that involves the forehead. Exam also reveals the finding shown above. Which of the following is the most appropriate treatment for this patient?
A) Acyclovir and prednisone
B) Ceftriaxone and vancomycin
C) Cephalexin
D) Prednisone
Answer: Acyclovir and prednisone
Herpes zoster oticus, also called Ramsay Hunt syndrome, is an otologic manifestation of herpes zoster. It occurs when there is a reactivation of varicella-zoster virus in the geniculate ganglion of cranial nerve VII (though other cranial nerves, including VIII and IX, may be involved). It presents with the classic triad of ipsilateral facial paralysis, pain in the ear and ear canal, and vesicles in the auditory canal and auricle. This form of Bell palsy is different from other forms as it has the characteristic skin lesions seen with herpes zoster. Contrast this to the skin lesion seen in Lyme disease (erythema migrans) or the absence of skin findings in idiopathic cases. Other common symptoms include altered taste, lesions on the tongue, and hyperacusis. The diagnosis can be made clinically with the classic presentation and rash. Treatment must include acyclovir, which improves outcomes. Steroids may be administered and might improve neurologic outcomes with mixed evidence. Complications of Ramsay Hunt syndrome include permanent neurologic dysfunction (facial weakness) and chronic neuropathic pain. Outcomes in Ramsay Hunt syndrome are generally worse when compared to other causes of Bell palsy.
Ceftriaxone and vancomycin (B) are antibiotics that can be used for more extensive skin infections, as this regimen covers for gram-negatives, gram-positives, and methicillin-resistant Staphylococcus aureus. It would be indicated if there was a superinfection in the setting of herpes zoster oticus. Cephalexin (C) is commonly prescribed for cellulitis, which presents with erythema, warmth, and tenderness over the skin. Prednisone (D), eye lubrication, and taping the eye shut at night is the appropriate management of a Bell palsy that is not clearly caused by herpes zoster. However, in the setting of an active herpes zoster infection, acyclovir should be given.
February
Image Source: Rosh Review
A patient presents after being bitten by a rattlesnake. Which of the following findings would be consistent with this envenomation?
A) Fasciculations
B) Respiratory paralysis
C) Slurred speech
D) Thrombocytopenia
Answer: Thrombocytopenia
Crotalinae envenomations can be caused by bites from snakes such as rattlesnakes, cottonmouth snakes, copperhead snakes, sidewinders, and water moccasins. The venom of a crotalid damages local tissues and leads to tissue destruction and can activate the coagulation cascade. Initial care should be focused on evaluating and irrigating the wound as well as removing any retained foreign bodies, such as fangs. If the wound cannot be explored, then a radiograph may be needed to rule out retained bodies. Incising the wound and attempting to suck out the venom is not indicated. Further care involves laboratory studies, including a CBC, chem-10, and coagulation labs. Laboratory derangements may include thrombocytopenia, a prolonged PT and PTT, a decreased fibrinogen, and an elevated D-dimer. The constellation of all these findings would suggest disseminated intravascular coagulation (DIC). The extremity should be examined and elevated. Care should be taken to evaluate for compartment syndrome, which presents with severe pain of the affected extremity that is worsened with passive range of motion of that extremity. Further management may require crotalid monoclonal antibody administration. Patients should then be admitted for observation and further care.
Fasciculations (A), respiratory paralysis (B), and slurred speech (C) are seen with Elapidae envenomations from snakes such as the coral snake. Coral snakes release a potent neurotoxin, and often the bite is minimally painful. Life-threatening sequela includes respiratory failure requiring intubation.
Looking for more practice questions? Put your knowledge to the test with this FREE shelf exam practice quiz of the most commonly missed shelf questions from the Rosh Review Shelf Exam Qbanks (one for each specialty)!