How to Survive and Thrive in Your Core Clerkships
- by
- Dec 10, 2021
- Reviewed by: Amy Rontal, MD

13 key tips to help you be successful (and avoid getting overwhelmed) in your clinical rotations.
Introduction
Clinical rotations are an incredibly formative experience—a precious and finite time dedicated to learning what it means to become a physician. Yet, the experience can be stressful and downright overwhelming. You will likely feel high pressure to impress your attendings and attain good grades. You may face competing demands, testing the limits of your time management and straining your personal life. Despite all of these challenges, the elements of success are straightforward and recognizable: a positive attitude, eagerness to learn, and willingness to put in the time and effort. Remember: although daunting, this is doable!
Your core clinical rotations, or core clerkships, generally consist of Internal Medicine, Pediatrics, General Surgery, Family Medicine, Neurology, Psychiatry, and Obstetrics/Gynecology—sometimes there will be an Emergency Medicine or Anesthesia core rotation as well. Most of these rotations are taken during third year, though a few may be taken in fourth year as well. A rotation at a specific clinical site may be as short as one week, or as long as twelve weeks.
For many medical students, third year represents a huge shift in mindset. Your schedule will transition from mostly studying and exams, to a much more hands-on experience spent with patients. Most students, after getting the hang of things, will vastly prefer third year to the preceding first and second years—this is because clinical rotations are an immersion into the real clinical practice of medicine.
Third year is an integral time when the proverbial light bulbs go “ding!” as the knowledge from your first two years is synthesized and reinforced in the context of helping real patients. You may form deep emotional bonds with patients and team members. And yes, along the way, you will be evaluated and graded—but please don’t let this be your only focus. And yes, sometimes third year can be a slog, and it’s okay to acknowledge that too. But, remind and recenter yourself often: you are here to acquire skills and knowledge that will be invaluable to your future as a physician. Seize this moment!
Let’s talk grades
Yes, I know we just discussed that there is so much more to life and clerkships than grades! But, since you are a hardworking medical student with goals and dreams, let’s talk grades—just for a little bit.
Let’s look at this survey of residency program directors, evaluating the most important academic and personal factors in selecting applicants for both interview and ranking. For “Education and Academic Performance Characteristics”, grades in required clerkships ranks 4th most important (4th most frequently selected) for deciding who to interview, and 6th most important for deciding who to rank. On first glance, this may be unimpressive—there are more important factors, right? Let’s think about this a little bit. The 2nd most important academic factor for both interview and ranking is the Medical Student Performance Evaluation (MSPE), sometimes colloquially referred to as the “Dean’s Letter”. This letter is meant to be a holistic summation of your performance throughout medical school. Realistically, the letter often relies heavily on clerkship performance, and will synthesize information from your clerkships including your grades (which will be described in a holistic narrative format) and sometimes selected quotations from your clerkship evaluations. As Step 1 of the USMLE becomes pass/fail, MSPE may well jump to being the most important factor! And the MSPE borrows from your clerkship performance.
If we switch to looking at “Personal Characteristics and Other Knowledge”, program directors selected letters of recommendation in specialty as 1st most important. Clerkships can be a valuable time to network and impress within your preferred specialty. If you perform strongly in a clerkship, you have just locked in a potential future letter writer!
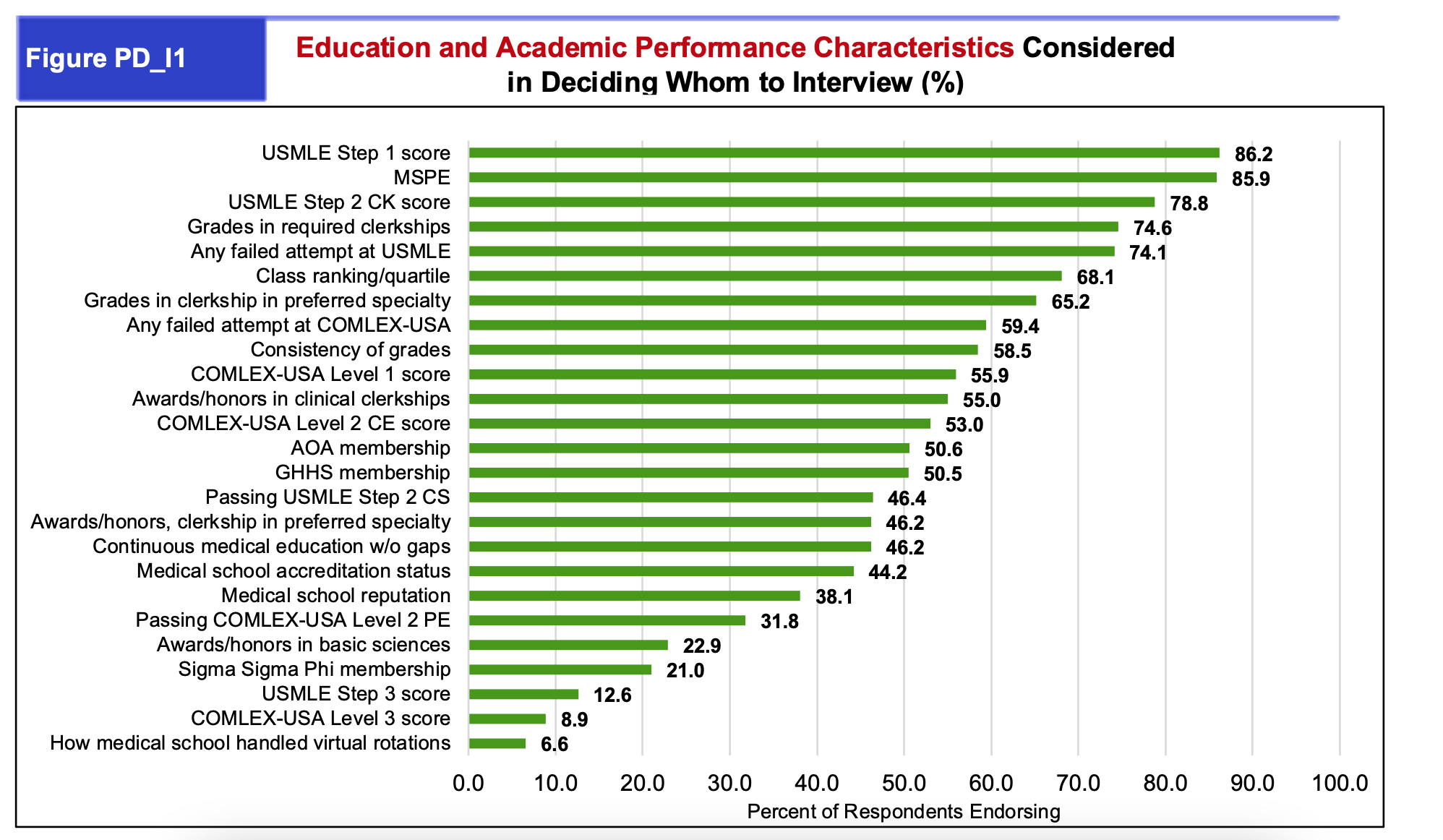
So, bottom line: clerkship performance—not just grades, but performance and written evaluations—are important for your residency applications. But keep in mind that for better or worse, the process is a long and summative one—so please don’t get hung up on a single grade or single evaluation. Note that in the academic factors chart, clinical clerkship grades were regarded as more important to program directors than an individual grade in a preferred specialty. Program directors are often interested in evidence of long-term good performance—which means you have plenty of opportunities to do well!
So, yes, your performance on clerkships will be a focal point in your residency applications. But, I encourage you to send your grades to the backseat, and to let other motivations drive you: to take skillful and compassionate care of patients, to practice and learn, and to become a great doctor! If you work hard and perform well with these goals in mind, your grades should follow.
Onto the advice!
1. Have a positive attitude
I cannot overstate this: a positive attitude is truly the crux of succeeding in your clinical rotations.
Be nice. During this time, you will be interacting with a deluge of new people—which is great! New patients, residents, attendings, nurses, techs, custodial staff, rotation coordinators, etc. Your patients and your team members will come from different walks of life. This will sound pretty simple: be nice to everyone. Please & thank you go a very long way.
Be enthusiastic. Be the kind of person you would want to work with in the future! Don’t groan when being assigned a new task or a new patient. Show your eagerness to learn from each new experience.
Show initiative. Volunteer to help out. Do the tedious-but-necessary task, especially if it benefits the patient. Read and learn about your patient’s diagnoses, without anyone telling you to do so.
Be the kind of person you would want to work with in the future!
Hone your interpersonal skills. Exercise common sense and do your best to read the room. Also, your attendings and residents are human—get to know them! Find out how they got on their current path.
2. Be respectful & professional
The basic aspects of professionalism include showing up on time, being prepared, and working with integrity. Your team members will notice if you are frequently late, or worse, “missing” without explanation. It will be evident if you cut corners or shirk tasks.
Be a team player. You will be interacting in close quarters, often one-on-one, with your fellow classmates. This is absolutely not the time to “gunner” your way to the top. Do not try to show up your classmates—your success should never depend on making someone else look bad. You will shine brightest if you demonstrate that you have a great team mentality and can work well with others. Again, remember, you are being evaluated not as a student, but as a future coworker – would someone be excited to work beside you based on how you’re engaging with conversations? Also, remember that your fellow medical students may be your greatest resource!
“Don’t be an asshole”. Keep your filter on at all times. Humor is a wonderful way to strengthen bonds and professional relationships—but it’s best to keep the humor lighthearted and non-personal. Don’t make fun of patients, team members, or staff. Avoid offensive or derogatory statements, in any context. If in doubt, cut it out! It’s better to be quiet than to be rude!
Be engaged and present. Keep phone time to a minimum when interacting with others. Do your best to remain engaged on rounds. Do not post about patients or team members on social media. It can be illegal, or at least highly inappropriate, to post identifying information about patients on social media.
Medicine is a small community—you never know who you’ll meet, and how they’ll cross paths with you again! Maybe your resident will be your future attending; maybe your attending will personally know the program director at your future dream program. Don’t be nervous—the easiest thing you can do is just be respectful to everyone you encounter!
3. Be empathetic
Be sensitive. Remember that patients are real people, and that being a patient places them in a vulnerable position. Sitting and listening can be incredibly meaningful to a patient or their family member. Become comfortable with using empathetic language, especially in difficult situations (e.g., ”I can’t imagine what you must be going through. I’m sorry that this is happening”). You can be a calming presence even during times of great fear or tension.
Simple acts of kindness, like getting a patient juice, or helping a tech make a bed, can make the day feel kinder and lighter.
Patients can be “cranky” or “difficult” at times—realize that they may be scared or angry about their situation. They may have prior experiences that have resulted in a distrust of medical care. Oftentimes, it’s not personal. Sometimes, a language barrier or a cultural barrier may impact your ability to connect with a patient. It’s worthwhile to read more about culturally competent medicine.
The hospital is a very stressful environment! Don’t resent your resident if they are too busy to answer your question in the midst of rounds. Don’t take it personally if the nurse is a little bit curt. You don’t know what they might be going through.
We’ll discuss further, but this advice does not mean that you ever should tolerate actual abuse. You never deserve to be abused, humiliated, harassed, or belittled—by patients or by staff. Rather, the advice just means that you should cut people a little slack when they’re stressed out—you’d want the same done for you!
4. Be prepared
Being prepared will make a huge difference in how you start each rotation, and start each day.
Read about the clerkship requirements in advance. Know when and where to show up, and clarify with the course director if you have any questions.
Pre-round every morning on inpatient rotations. Give yourself ample time to do this so that you don’t feel rushed. Look up your clinic patients the night before for outpatient rotations. Read about their diagnoses if you have the time. You’ll feel more at ease if you have a good handle on your patients for the day.
If you are helping out with a procedure or scrubbing into a case, read about the relevant anatomy, and even watch videos of the procedure or surgery if you can.
5. Work hard
Put in the time and put in the effort. You will get out what you put in. Work hard, and don’t cut corners. Spend time on your presentations. Spend time on your notes.
Go beyond the bare minimum. Increase your responsibility once you feel proficient. Be proactive! For example, after you have discussed with your resident, you can ask to call a consult on a patient that you understand well.
Sometimes, working hard involves more “menial” or tedious tasks (I don’t mean getting your residents coffee every morning, which is not your responsibility). You may need to obtain outside records or wait on hold with a scheduling line. You can gripe about the frustrations and inefficiencies of the healthcare system, yet you must still do your best to work within it. Ultimately, remember that you’re doing it to help the patient! Coordinating care can be the difference between another few days in the hospital, so it can mean a lot.
Get a feel for when the “appropriate” time to leave is, which can be tricky to navigate—and oftentimes there’s no right answer. The appropriate time to leave each day varies greatly by rotation and by team. On an inpatient rotation, you should generally stay until you have been assigned all of the potential new patients you would get that day, and have completed all necessary tasks and required notes that day. In practice, even if your work is done, you may want to not leave too early—being present means that you will have more chances to observe and interact with the rest of the team, or to learn updates on your patients. If it’s busy, there may be interesting things to learn about other patients on the service. You don’t want to be perceived as the medical student who is never there! Conversely, residents will get too busy to realize they are keeping the medical student late. The question, “can I help with anything?” at the end of a day generally implies asking to leave—and it’s okay to ask, if at a reasonable time!
Fill your time. Sometimes, there can be a lull between new inpatient admissions, or a no-show in clinic. While you should feel free to breathe a little, or have a snack, don’t idle too long! This is a great time to read and learn about your patients. Go on UpToDate, peruse the literature, and do a deep dive. Pro-tip: these lulls are also a great time to study! Bring a book or tablet with you. The more you can fit in studying at work, the more time you’ll have after you get home! Bonus: you’ll look productive the whole time.
6. Cherish this time
Your clerkships are a special time and uniquely protected for learning. You are heavily supervised with significantly reduced responsibilities compared to residency and beyond. You have the freedom to ask questions, not know answers, and make plenty of mistakes!
It is a true honor and privilege to care for a patient. They have placed their trust in you and the rest of the care team during a vulnerable time. Clerkships can be a dramatic change from standardized patients or case scenarios in a question bank. Treasure the sacred fact that a patient, a real human being, has opened up to you during their time of need.
On an inpatient clerkship like internal medicine or pediatrics, medical students have more time than other members of the care team to spend on each individual patient. Spend time at the bedside! Get to know the patient. Talk to their family members. Ask them stories about their life and their experiences. Where did they grow up? Where have they traveled? How did they meet their spouse? Your interactions with patients may range from heartwarming to emotionally exhausting—this is the realness of life, of medicine, of patient care.
Think of this time as a “sandbox” where you can practice becoming a doctor in a bunch of different specialties. If you are undecided about a specialty, this can be a great time to try on new hats. You may work with new role models and become inspired. Find out how your attendings got on their career paths, which can be insightful even if not in your desired specialty. Even if you’re on a rotation that couldn’t be farther from your desired specialty, realize that you may still learn valuable and highly applicable medical knowledge. Radiologists and pathologists must understand clinical disease states. Many internal medicine subspecialties will interface closely with surgeons. Many specialties have both an inpatient and outpatient component. You can pick up broadly translatable skills: increasing your efficiency with tasks, notes, and presentations will facilitate a smoother transition to residency.
Even though you will be heavily supervised, your actions can still be impactful. Your notes will actually enter the patient record—and often be readable by the patient. Consultants and other doctors will read your notes too, often before the attending attests it. Your patient will remember things that you say, so speak carefully. If you help suture a real wound, that patient’s scar will heal with your aid. With great power comes great responsibility–your power and responsibility will continue to grow considerably with each next step in training. Always ask for help when you are uncertain!
7. Growth mindset
Clerkships require a big mentality shift. Remind yourself that rotations are a critical time to learn clinical medicine, where you can ask questions and make mistakes. It’s expected that there are many, many things you don’t yet know—that’s normal, and that’s why you have to learn! When you don’t know the answer to a question, don’t beat yourself up! Just be kind to yourself, and let it motivate you to learn.
You should—and deserve to—receive feedback, ideally frequently and thoughtfully. So long as the feedback is delivered to you respectfully and constructively, do your best to gracefully accept it with an open mind. Don’t get defensive. Appreciate that someone deliberately took time out of their busy schedule to think about your performance, sit down with you, and encourage you to strive for your potential. Use feedback as an opportunity to better yourself. You’ll find that the most helpful feedback is specific and actionable. For example, if an attending asks you to ensure that your presentation structures maintain the SOAP order, be mindful of this the next time you present! If you have the opportunity to work with a single attending for an extended period of time, do your best to integrate the feedback quickly—they’ll notice!
You should feel empowered to ask for feedback, just do so considerately. Don’t demand feedback so frequently that you interrupt the flow of your team’s workflow.
When you ask for feedback, it can be helpful to refer to a specific aspect and in a timely way (“Do you have any feedback on the structure and flow of my presentations this morning? After you have a chance to read the two H&Ps I just signed, could you please let me know what suggestions you have to strengthen the history/summary statement/problem list/etc.?”)
Occasionally, you just won’t jive with a team member. Sometimes, it’s not you, and it’s not personal. That’s life—while it feels kind of crummy, it happens! Keep your head up, it’ll be alright as long as everyone treats each other respectfully and professionally. A big part of your career entails working well with other people, and that includes all types of different personalities!
8. Ask for help
When in doubt, ask! You are not expected to know everything. While imposter syndrome is real, the whole point of school is that you are very much still learning. You’ll find that your residents and attendings are still constantly learning as well.
You may have heard the phrase “you don’t know what you don’t know”, and also, “the more you learn, the less you know”. Even the most knowledgeable medical students are limited by the bounds of their experience. Don’t overstep the bounds of your knowledge—overconfidence can lead to inappropriate or dangerous situations!
It’s completely okay to express nerves or discomfort. Don’t “go rogue” or act independently without discussing with your team members. Avoid sharing bad news or starting a goals of care discussion on your own. Don’t explain anything to a patient that you don’t understand. It’s perfectly acceptable to tell a patient that you are a medical student in training, and that you will discuss with your supervising residents and/or attendings.
Don’t overstep the bounds of your knowledge—overconfidence can lead to inappropriate or dangerous situations!
Learn from those around you. Attendings, residents, nursing, social workers—everyone on the care team—can be great resources to learn about clinical medicine itself, but also the practice of medicine and the workflow of a hospital or clinic.
Ask your questions thoughtfully and try to time them considerately. It’s often fine to ask a quick clarification question on rounds, or to try and squeeze in a short question between patients. If the patient census is large, a complex question may be better saved for a lull later in the day. If the question is a general knowledge question, try to answer it by looking it up yourself first, then ask your remaining questions after you’ve made an attempt!
9. Practice & study
Practice makes you better!
For most students, oral presentations are difficult and unintuitive. You may marvel at how your senior resident concisely presents with very few notes, remembers lab values, etc. Or maybe you’ll notice your intern fumbling through their sheets—it’s a hard skill! It gets better with time, experience, and practice. You’ll need to practice the structure and flow of presentations before it becomes second nature. You’ll need to parse through hundreds of lab values before it becomes easy to pinpoint abnormal vs. normal range values. Practice going through the flow of a presentation multiple times.
Similarly, your entire workflow may seem intimidating: pre-rounding, presenting, writing notes, calling consults, following up on tasks! This too will improve with practice and experience. Anchor yourself—data gathering, information synthesis, and organizational skills will be valuable in many domains of your career, and even your personal life.
Study often, study early, and study hard! Your core clerkships will be accompanied by NBME shelf exams. You should study for the sake of learning the specialty, and ensure that the resources you are using are efficient and effective. Check out our post on the top resources Cram Fighters are using to improve their shelf study plans.
Every school and every rotation tends to have a different weight for the shelf exam in your clerkship grade—be mindful of this, but try not to let the grade be your driving factor. A lot of shelf exams overlap with each other, USMLE Step II, and USMLE Step III material—and, unlike some of the basic science esoterica on the USMLE Step I, a lot more of the shelf exam material is relevant to patient care! A lot of this material will travel with you throughout your medical training and your career beyond.
Bring study materials with you so that you can easily read a chapter or churn out a few practice questions during downtime! Start studying early on for each new rotation.
In addition to studying for your shelf exams, read about pathology as it comes up in real-time, with real patients. The knowledge will be more interesting and will stick much better when you can connect it to a real-world case. You will be more invested in learning disease pathophysiology and treatment when you need to explain a disease to a patient and their bedside care team.
10. Be flexible
Each new rotation may feel like Groundhog Day—just when you got the hang of the last rotation, you’re thrown into something new a few weeks later! It can be jarring to show up to a different place at a different time, with different people, and be held to different expectations. It’s difficult, but this adaptability is essential in medical training. The same thing will happen in residency—you’ll have to master a whole bunch of different rotations! Many attendings will gear-switch between clinic, the operating room, inpatient consults, and research—sometimes all in the same week—or even same day!
Each time you start a new rotation, stay humble and open-minded. Get a feel for your new rotation, your new team members, your new attending, your new expectations. You might feel like you’re fumbling around for the first week—that’s totally normal. General differences between specialties and workflows can guide you. For example, an oral presentation for a surgery rotation is generally expected to be more concise than an internal medicine one.
Even when you stay on the same rotation, a change in attendings can throw you off, as each attending may have different preferences about notes and presentations. Feel out your attendings and tailor your behavior and presentations for their (usually obvious) preferences. Your notes may impress one attending, but disappoint another! This inconsistency can be exasperating, but reframe: this is a learning experience, where you learn that there are thousands of different and stylistic ways to be a great doctor. Practice them all. Try out all these different suggested strategies, and pick which ones you want to integrate into your own future practice.
There is certainly subjectivity to your evaluations, and it may feel frustrating that there are human factors outside your control. But realize this—it’s subjective, but it’s not random. If you consistently demonstrate a positive attitude, work hard, and integrate feedback, you will improve. If you improve, your evaluations will follow suit!
11. Be deliberate about your time
Time management is the hardest skill, and there is no easy way to master this. It is generally helpful to use a calendar tool and to choose a system to keep track of your to-do’s and deadlines.
Make time for the things that matter, and block that time out in your calendar! The more efficiently you study at work, the more time you’ll have to relax at home. I would caution you to avoid unstructured “veg out” time. If you want to relax, block off time for it!
Unquestionably, with your busy schedule and the limited time in a given day, you’ll have to make sacrifices. Do you need to prioritize family, such as if you have a spouse or children? Will you use your day off to sleep, or will you feel more rejuvenated if you go out for drinks? There are no right answers—but be deliberate. Block off time for both work and play. For example, two hours of studying here, then an hour for family dinner there.
12. Know what’s expected of you
You are primarily expected to learn, not to be a workhorse. Think about it this way: if you weren’t there, the residents and attending should still be able to handle the inpatient service, perform a surgery, or hold a clinic visit—even in your absence. Yes, it might make you feel a little superfluous, but that’s because you’re there to learn! You are not there to replace a resident. Similarly, you are not required to run errands for the team (but if you were going on a coffee run anyway, you could be a team player and ask if anyone wants anything—make sure the residents pay you back!).
As you become increasingly proficient at clinical medicine and learning your workflows, you may be able to alleviate some of the shared burden of the team’s work—that’s great! Learning by doing is fundamental to your growth. Just be mindful that your primary objective is to learn. Even if you’re a highly efficient and competent medical student, you may find that diving deep and learning thoroughly about a patient can be more valuable to your growth than simply taking on more patients.
You are expected to work with integrity, and to follow through. If you are assigned a few reasonably-sized tasks (e.g., clarify a medication dose, communicate with a nurse, and call a medical records office), you are generally expected to attempt and complete them all to the best of your ability. If you are asked to discuss a few key differential diagnoses, make sure they are present in your note.
Communicate. If you have an important commitment, difficult situation, or medical issue, it is often best to discuss with the clerkship director and coordinator upfront. Use your discretion and judgment for what is appropriate to share and when. While you are entitled to your privacy, there are advantages to being a little vulnerable with your residents and attendings. For example, if your family member is experiencing a serious medical issue, you may find it hard to focus, or be checking your phone often—your team may wonder why you seem “checked out” and could interpret this as apathy. But if you are willing to share a bit of information, they may be empathetic—it’ll make a lot more sense to them why you need to run out and take a phone call during rounds. For certain social commitments such as weddings, you’ll want to carefully review your clerkship and school policies before making travel plans.
Know what’s expected of others
You will meet amazing people. You’ll work with aspirational attendings who are kind hearted and supportive, who teach you clinical pearls that you’ll commit to lifelong memory, and even occasionally bring you tasty breakfast. There are residents who will carve time out of their busy schedules to patiently coach you before a presentation or teach you to call a consult, or prepare an entire chalk talk to educate you on your patient’s disease. There are nurses who will warmly show you how they place IV or change a dressing. There are custodians who will walk with you the entire route when you’re lost in a convoluted hospital. Show these amazing people your appreciation—kindness makes the world a better place.
Hopefully, you will work with zero, or at least very few, “baddies”. You deserve to be treated with respect. Always. We discussed that sometimes people are stressed out and busy, and may be a bit curt or not have ample time for you—that’s life. You never deserve to be bullied, harassed, belittled, humiliated, or abused. You never deserve to be insulted based on your race or gender. Feedback should be about your observable work and behavior, not who you are as a person. Talk to your clerkship or school administrators if you have concerns about being mistreated. Think about this: even if you deliver the most lackluster oral presentation, the appropriate forum would still be the attending providing respectful and constructive feedback in a private setting—not being mocked or berated.
Even when your team is very busy, you deserve deliberate time dedicated to teaching. Your attending or senior residents should make the time for you.
13. Be kind to yourself
This process is hard, and can feel exhausting, stressful, and thankless. You may feel overwhelmed even if you are treated with utmost support and respect. That’s a normal feeling. Medical school is hard. Clinical medicine is hard!
Take care of yourself. Try to sleep. Try to make time for self-care. Remember to eat. Bring snacks!Talk to friends, loved ones, and fellow classmates. It’s okay to be vulnerable. It’s okay to say that you’re struggling. You may be surprised—and somewhat reassured—to learn that others are struggling too.>Keep perspective. Residency is stressful, too; medical training is a long and difficult journey. Focus on what you can control. Keep your growth mindset, and focus on learning and constructive self-improvement. Focus on helping your patients.
Grades are not everything. Even the residency match is not everything. There are so many routes to attain a meaningful career in medicine.
You matter. Don’t lose yourself in the process of medical school. Nothing is worth your happiness or your life. It’s never a bad time to check out our mental health check in blog.









