Preparing for Step 2 is a huge milestone—congrats on making it this far in your medical training! You’ve survived clerkships, grown through real patient encounters, and now you’re gearing up for an exam that truly tests your clinical reasoning. And here’s the truth: Step 2 practice questions are one of the most powerful tools you have. Working through Qbanks forces you to apply what you’ve learned in a way that actually sticks, setting the foundation for long-term mastery and a score you’ll be proud of.
That said, it’s important to approach Step 2 questions strategically. You’re a busy med student with zero time to waste, so the way you use practice questions matters just as much as how many you get through!
In this guide, we’ll break down the five major question types, walk you through how to tackle each one, and explain what makes the correct answer the best answer. We’ll wrap up with high-yield test-taking strategies to help you walk into exam day with confidence.
Let’s start by looking at what makes Step 2 questions a little different from what you’ve seen before.
Preparing for Step 2? Meet Blueprint’s combined Step 2 & Shelf Exams Qbank with 5,500+ practice questions that most closely match what you’ll see on your USMLE Step 2 and all of your shelf exams. Get started with a 7-day free trial!
Why Step 2 Practice Questions Require a Different Approach
You might be tempted to approach Step 2 the same way as Step 1, but it’s a different beast. Step 1 focuses heavily on basic sciences: memorization, pathways, and isolated facts. Step 2, on the other hand, is all about clinical reasoning, decision-making, and patient management. You’re not just recalling information anymore. You’re applying it to clinical scenarios.
Some key differences between Step 1 and Step 2 include:
1. Step 2 has a clinical focus with real-world presentations, not ideal scenarios.
Real patients don’t always fit the textbook, which makes Step 2 questions more difficult because the questions stems aren’t idealized scenarios like they are in Step 1. While Step 1 is like listening to a clear station with just the main melody, Step 2 feels more like static on a radio with question stems often including extra details, comorbidities, and red herrings.“Buzzwords” are also less common in Step 2.
2. Step 2 has longer question stems.
Vignettes can be lengthy and detailed, mimicking real patient encounters. It’s crucial to sift through information efficiently and not lose sight of the big picture. Always approach the stem strategically and read the question first, then skim the stem for context and key details.
3. You need to go beyond memorizing and demonstrate clinical readiness.
Step 2 focuses on what’s best for patient care, rather than recalling every detail from a text book. The rote memorization of isolated facts, Anki cards, or buzzwords that may have carried you through Step 1 won’t be beneficial. Step 2 challenges you to develop your own decision-making frameworks and flowcharts for clinical management, guiding you through patient care scenarios in a logical, stepwise way.
4. More material, more to know.
Step 2 tests on a broader range of topics than Step 1, covering clinical knowledge across all specialties. You’ll need to be familiar with the diagnosis and management of common and uncommon conditions, preventive care, and complications and side-effects, which makes the exam both wider in scope and more applied. Make sure to allocate enough time in your study schedule for content review, spaced repetition, and question banks.
Understanding these differences between Step 1 and Step 2 early on will help you adjust your study strategy and approach questions in a way that maximizes your score!
Step 2 Practice Questions: How to Approach Each Question Type
Step 2 CK includes a variety of question types to test different clinical competencies. It’s important to recognize the style of question first and tailor your approach accordingly.
Here are the different question types you’ll encounter during Step 2:
1. Diagnosis Questions
Diagnosis-style questions ask you to determine the most likely condition based on a patient’s history of present illness, symptoms, risk factors, physical exam findings, labs, and imaging. Sometimes the answer choices list specific diseases (e.g., pulmonary embolism), while other times they ask about the underlying mechanism, associated clinical feature, or a downstream complication (e.g., right ventricular hypertrophy). Your goal is to create a differential diagnosis and select an answer that best fits the scenario.
Sample Question
A 32-year-old woman presents with sudden-onset shortness of breath and sharp, pleuritic chest pain that began an hour ago. This morning she arrived from a flight after a business trip in Tokyo. Her heart rate is 118/min, respiratory rate is 26/min, and oxygen saturation is 90% on room air. Lung exam is clear. EKG shows sinus tachycardia. Which of the following is the most likely diagnosis?
A) Panic attack
B) Community-acquired pneumonia
C) Pulmonary embolism
D) Spontaneous pneumothorax
Explanation
Sudden dyspnea, pleuritic chest pain, tachycardia, prolonged immobility during a long flight is the classic clot setup making pulmonary embolism (choice C) the correct answer.
How to Approach Diagnosis Questions
Start by summarizing the case with a “one-liner.”
What is the patient’s key symptom, timeline, and risk factor?
Consider the time course.
Rapid vs. gradual onset can significantly narrow the differential.
Identify the pertinent positives and negatives.
These high-yield details steer you toward one diagnosis over another. Pertinent positives: sudden dyspnea + pleuritic chest pain + sinus tachycardia + long flight. Pertinent negatives: no fever or lung crackles (rules out pneumonia) and no mention of absent lung sounds (rules out pneumothorax).
Most likely diagnosis: C) Pulmonary embolism.
While Step 1 often emphasizes buzzwords like the S1Q3T3 EKG pattern, Step 2 is more focused on the most likely clinical presentation, in this case, sinus tachycardia. In other words, the absence of a classic “buzzword” should not be a reason to rule out an answer choice.
2. Management Questions
These questions focus on the sequential care of a patient and often require you to distinguish between diagnostic evaluation and therapeutic intervention (e.g., imaging, endoscopy, pharmacotherapy, or surgery).
Below are the three major formats you’ll encounter:
2A. Next Best Diagnostic Step
This applies when the patient’s presentation supports a broad differential and you need additional testing to narrow it.
Sample Question
A 46-year-old woman presents with a new, firm, nontender mass in her left breast that she noticed 2 weeks ago. It does not fluctuate with her menstrual cycle. She has no personal or family history of breast cancer. Your physical exam confirms a 2-cm irregular, fixed mass in the upper outer quadrant of the left breast. No skin changes or nipple discharge are present. What is the next best step in diagnosis?
A) Breast ultrasound only
B) Diagnostic mammogram
C) Breast MRI
D) Fine-needle aspiration without imaging
Explanation
In a woman over age 30 with a palpable breast mass, the next best diagnostic step is a diagnostic mammogram (choice B). Ultrasound is an appropriate answer choice for women under the age of 30. MRI is reserved for high-risk populations or when mammogram/US are inconclusive. FNA is not first-line when appropriate imaging has not yet been done.
2B. Next Best Treatment Step
These questions ask what will stabilize the patient right now, not what is part of long-term or downstream management.
Sample Question
A 62-year-old woman presents with sudden, severe substernal chest pain radiating to her left arm. She is diaphoretic and nauseated. Vital signs: BP 88/54 mm Hg, HR 52/min. ECG shows 3-mm ST elevations in leads V2–V5. What is the next best step in management?
A) Start metoprolol
B) Give sublingual nitroglycerin
C) Begin high-intensity statin therapy
D) Activate the cardiac catheterization lab
E) Obtain serial troponin levels
Explanation
This patient has an anterior STEMI with hypotension, and the priority is reperfusion. The correct next step is activation of the cardiac catheterization lab for emergent PC (choice D). Aspirin, beta-blockers, statins, and troponins are part of MI management, but none stabilize the patient right now.
2C. Next Best Medication
These questions focus on the most appropriate pharmacologic therapy after establishing the likely diagnosis.
Sample Question
A 28-year-old woman comes in with irregular menstrual cycles, acne, and increased facial hair. BMI is 32 kg/m². Pelvic ultrasound reveals enlarged ovaries with multiple peripheral follicles. The pregnancy test is negative. She is not currently trying to conceive. Which medication is the most appropriate to alleviate symptoms?
A) Metformin
B) Leuprolide
C) Combined oral contraceptive pill
D) Clomiphene citrate
Explanation
The patient has classic PCOS. Since she is not trying to conceive, the next best pharmacologic step is a combined oral contraceptive pill (choice C), which regulates cycles, lowers androgen levels, and improves acne and hirsutism. If stimulating fertility is desired, clomiphene citrate can be used as first-line therapy to stimulate ovulation.
How to Approach Management Questions
Identify whether the question requires a diagnosis, treatment, or medication.
Reading the last line of the question stem first often helps.
For diagnostic next steps…
Choose the test that gives the most immediate and actionable information that’s age appropriate.
For treatment next steps…
First, decide if the patient is stable or not stable. Stabilization always overrides testing or long-term therapy.
In high-acuity scenarios…
Think about what will keep this patient alive in the next 10 minutes? Reperfusion, airway support, fluid resuscitation, and hemorrhage control are common answers.
For medication questions…
Pick the first-line drug that best addresses the patient’s goals (symptom control vs fertility vs prevention).
Don’t get distracted by long-term management options.
Step 2 wants sequence, not a list of everything you’d eventually do. If two answers seem correct, pick the one that occurs sooner in the clinical timeline.
3. Prediction Questions
These questions ask you to identify a patient’s most likely diagnosis then go a step further and pick the correct associated prognosis, complications, or treatment related to that diagnosis.
3A. Most Common Cause of Death/Prognosis:
These questions test your knowledge of what typically is the outcome for a disease trajectory.
Sample Question
A 19-year-old man presents with progressive difficulty walking and frequent falls that started in early adolescence. On exam, he has dysarthria, absent lower extremity reflexes, and an ataxic gate. Laboratory studies reveal impaired glucose tolerance. Genetic testing confirms a GAA trinucleotide repeat expansion on chromosome 9. Which of the following is the most likely pathophysiologic process that may contribute to his premature death?
A) Respiratory muscle weakness
B) Hypertrophic cardiomyopathy leading to heart failure
C) Recurrent aspiration due to dysphagia
D) Severe diabetic microvascular complications
E) Cerebellar degeneration
Explanation
This patient presentation points to Friedreich’s ataxia. In Friedreich’s ataxia, while neurologic decline is prominent, cardiomyopathy leading to heart failure (or arrhythmia) remains the most common cause of death. Therefore, answer B is most likely.
3B. Most Likely Complication Following an Intervention/Procedure
These questions ask what problem is most likely to occur during the course of an intervention or after a procedure.
Sample Question
A 48-year-old woman underwent a laparoscopic cholecystectomy 8 months ago for symptomatic cholelithiasis. She now presents with progressive painless jaundice, dark urine, and pale stools. Laboratory studies reveal elevated direct bilirubin. What is the most likely cause of her current presentation?
A) Retained gallstones in the common bile duct
B) Bile duct stricture due to surgical injury at time of cholecystectomy
C) Primary sclerosing cholangitis
D) Viral hepatitis
Explanation
The patient’s presentation indicates obstructive jaundice pathology. Given the delayed timeline and presentation, a bile duct stricture from prior surgical injury is most likely (choice B).
3C. Most Likely Side Effects of a Medication
These questions focus on common, clinically relevant adverse effects after starting a medication.
Sample Question
A 32-year-old woman presents for follow-up after being started on a long-term medication for recurrent episodes of mania and depression. She reports mild fatigue, weight gain, and constipation over the past few months. On exam, her thyroid gland is slightly enlarged but nontender. Laboratory studies reveal an elevated TSH with low-normal free T4. Which of the following medications is most likely responsible for her current laboratory findings?
A) Valproate
B) Lithium
C) Carbamazepine
D) Fluoxetine
E) Risperidone
Explanation
The patient has a history of bipolar disorder and the clinical scenario describes long-term lithium therapy. Lithium commonly causes hypothyroidism with elevated TSH, low/normal free T4 (choice B).
How to Approach Prediction Questions
Lock in the diagnosis first
These are typically second-order questions. Use the scenario to narrow your differential before thinking about complications or management.
Pay attention to key words.
Watch out for “most common,” “likely,” or “frequent.” Step 2 favors real-world patterns over rare exceptions.
Use context clues.
Age, timing, and risk factors matter. Post-op complications differ by how long after surgery the patient presents. Think “timeline & probability.”
4. Primary Care: Disease Prevention and Surveillance Questions
For these questions you’ll often be asked not just to diagnose or treat, but also how and when to screen, monitor, or counsel patients to prevent disease.
Here are some question types to be ready for:
4A. Healthcare Maintenance
These questions often test the USTFP guidelines that you’ve studied for your Family Medicine and Adult Outpatient Medicine shelf exams.
Sample Question
A 62-year-old man comes for routine follow-up. He has a 45 pack-year smoking history but quit 5 years ago. He has no respiratory symptoms or known lung disease. Which of the following is the most appropriate next step regarding lung cancer screening?
A) No screening needed since he’s asymptomatic and quit smoking
B) Recommend annual low-dose CT scan of the chest
C) Chest X-ray now and in 1 year
D) Sputum cytology yearly
E) Routine lung cancer screening is not recommended
Explanation
Guidelines recommend annual low-dose CT for adults aged 50–80 with a 20+ pack-year smoking history, who currently smoke or quit within the past 15 years (choice B). Even if the patient quit recently, the elevated risk still warrants screening. Chest X-ray and sputum cytology are not recommended for screening.
4B. Normal/Abnormal Development
These questions are most commonly seen when pediatric and OBGYN knowledge is tested. You need to master the normal presentation of labor, development, and more to be able to determine when something is abnormal.
Sample Question
A 9‑month-old infant is brought to the pediatric clinic for a well‑child visit. On exam, the infant does not yet roll over in either direction, smiles, has a good pincer grasp but cannot wave hello, and only says mama. Which of the following is true about this infant’s development?
A) There is no concern, all of these findings are expected at this age.
B) Lack of rolling over is a concern requiring further motor development evaluation.
C) Lack of speaking 10+ words is concerning and warrants evaluation of a speech delay.
D) Not being able to wave hello is a concern and is expected at this age.
Explanation
By 9 months an infant should typically be able to crawl and pull to a stand, have a good pincer grasp, and say mama/dada (choice B). Speaking 10+ words and waving develops around 1 year.
How to Approach Health Maintenance Questions
Recognize the guideline being tested.
Most Step 2 preventive questions are about age, risk factors, or timing for screenings, vaccinations, and developmental milestones.
First, master what’s normal.
Only then can you recognize what’s abnormal!
5. Ethics, Patient Safety, and Biostatistics
Finally, the last type of questions are in the broad social sciences category. The best way to approach these is to review the content and do as many practice questions as you can.
Here are some examples:
5A. Ethics and Professionalism Questions
These test your ability to navigate patient autonomy, informed consent, confidentiality, and decision-making capacity.
Sample Question
A 72-year-old man is admitted for acute exacerbation of chronic obstructive pulmonary disease. After several days of hospitalization, he refuses intubation and mechanical ventilation if his breathing worsens, stating that he values quality of life over prolonging life with invasive measures. He has no advance directive on file. On examination, he is alert, oriented, and fully capable of describing the risks and benefits of intubation. He clearly states that he does not want life-sustaining treatment and does not wish to discuss changing his mind. Which of the following is the most appropriate next step in management?
A) Proceed with intubation against his wishes.
B) Seek a court order to appoint a medical guardian.
C) Respect his decision and document his wishes in the medical record.
D) Admit him to psychiatry for further evaluation.
Explanation
The patient is competent and fully informed, and has expressed a clear refusal of life-sustaining treatment. Competent patients have the right to refuse medical interventions, even if refusal may result in death. Intubating against his wishes, seeking a court order, or psychiatric admission is unnecessary and unethical. Therefore, the answer is C.
5B. Patient Safety/Quality Improvement
Patient safety and quality improvement questions test your understanding of system-based practices that reduce errors, improve communication, and enhance overall healthcare delivery.
Sample Question
A 67‑year-old man is admitted for community‑acquired pneumonia. On day 2 of his hospital stay, a first‑year medical student reviewing the medication administration record notices that the patient missed two doses of his scheduled antibiotic, once on the evening shift and once on the night shift, with no documented reason. The student considers reporting this to the team but is unsure whether it’s “their place.” No one on the team seems aware of the missed doses. Which of the following interventions is most likely to improve communication and prevent missed medication doses on this unit?
A) Hold daily interdisciplinary “safety huddles” at the start of each shift.
B) Replace verbal hand‑offs with written notes only.
C) Allow only senior staff, not students, to report medication discrepancies.
D) Reduce antibiotic frequency from BID to once-daily to reduce dosing errors.
E) Delay all medication scheduling until attending physician review.
Explanation
Frequent communication failures especially during handoffs and shift changes are a major source of preventable medical errors. Safety huddles provide a regular platform for nurses, physicians, pharmacists, and other staff to highlight missed doses, reconcile medications, and collaboratively plan care (choice A).
Other options are less effective or potentially unsafe. Limiting reporting to senior staff (C) discourages the open communication culture needed for safety. Reducing the antibiotic frequency (D) may not be clinically appropriate. Delaying medications (E) risks undertreatment. And replacing verbal handoffs with only written notes (B) may worsen miscommunication given the complexity of inpatient care.
How to Approach Patient Safety/Quality Improvement Questions
Recognize when the question is about systems and team processes.
Quality improvement is not just about individual patient management. It often revolves around communication, handoffs, rounds, or error prevention.
Think “what system change reduces error risk?”
Options often include checklists, structured rounding, huddles, and standardized communication protocols. Prioritize team‑wide, system-based changes that are highly reliable. Don’t depend on chance or memory. Beware of “fixes” that compromise care quality or individual responsibility. Reducing dosing frequency or delaying therapy are usually distractors.
Finally, consider inclusivity.
Tools that encourage even junior staff to speak up often improve safety culture.
5C. Biostatistics
You’ve seen these questions on Step 1 and they’ll also be on Step 2.
Sample Question
A 55-year-old man presents for evaluation of chronic cough. His physician orders a new rapid test for tuberculosis (TB) that has a sensitivity of 90% and a specificity of 95%. The prevalence of active TB in this patient’s population is less than 1%.Which of the following statements is most accurate regarding the interpretation of a positive test result in this patient?
A) The positive predictive value is very high because the test has excellent specificity.
B) The positive predictive value is low because the disease is uncommon in this population.
C) The negative predictive value is low due to the high sensitivity.
D) Sensitivity and specificity change depending on the patient’s age.
Explanation
PPV depends on disease prevalence. The positive predictive value is low because the disease is uncommon in this population (choice B). Even with high sensitivity and specificity, a rare condition will have a low probability that a positive result truly indicates disease. Sensitivity and specificity are intrinsic to the test and don’t change with age.
Building a Study Plan That Incorporates Step 2 Practice Questions
Creating a structured, personalized study plan will help you do well on Step 2.
Here’s some tips that’ll help you crush it on exam day:
1. Start early!
There’s a lot of material to cover, and you simply can’t memorize every detail. Instead, give yourself time to practice learning how to think clincially and recognize patterns across different scenarios. Starting early also gives you room to experiment with different study strategies, see what works for you, and adjust your plan as you learn more about your strengths, weaknesses, and how you best retain information.
2. Take a baseline test, and set a goal.
Start by taking a full-length practice exam to see where you currently stand. Use this baseline to guide how you allocate study time and which areas need the most focus. I’ve seen students start with a 210 on their baseline practice test and jump all the way to 260 by test day! Remember, your starting score is just a starting point, it’s not your final destination.
Below is the average Step 2 score published by the National Resident Matching Program for every speciality. This will give you a good sense of what your goal score should be.
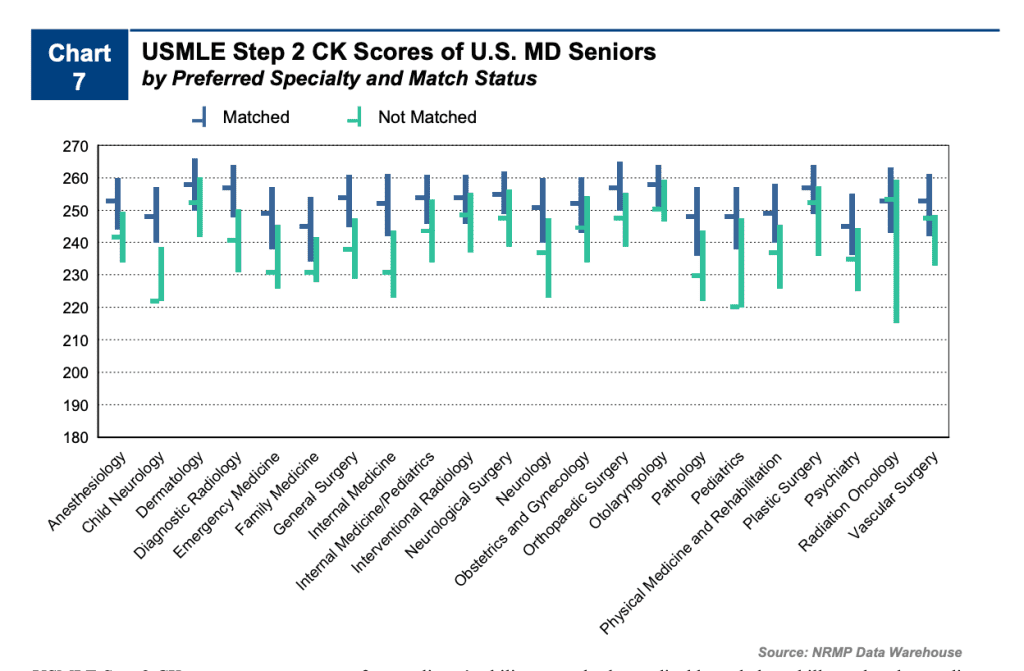
Source: NRMP
Check out this post on Step 2 percentiles to break down your Step 2 score and what it means!
3. Incorporate content review, spaced repetition, and question banks.
Blend reading, videos, or notes with active practice using question banks. You’ve learned a lot during clinical rotations. Whether it’s Anki, the whiteboard method, or something else, pick a retention strategy and spaced repetition method that works best for you. It’s also important to practice applying this knowledge to exam-style question stems.
4. Be consistent, and practice regularly.
Short, focused study sessions every day are more effective than occasional marathon sessions. Regular practice helps reinforce concepts, improve recall, and build stamina for long exam blocks. The average dedicated period for Step 2 is four to six weeks, so aim for doing approximately 60-100 Step 2 practice questions a day.
5. Study well during clerkships and for shelf exams.
Take advantage of clinical rotations to connect real patient experiences to your studying. Observing presentations, management decisions, and outcomes in real time will make Step 2 material more intuitive and easier to remember. Learn the content well for your shelf exams. The better you understand it now, the smoother Step 2 will feel later.
Step 2 Test-Taking Strategies
Step 2 isn’t just about what you know, it’s also about how you approach questions.
Here are some tips that can really help on exam day:
1. Have a routine.
Develop a method for tackling every question and stick to it. Whether it’s underlining key details, mentally summarizing the patient, or running through your differential, having a repeatable process keeps you organized and confident.
2. Read with purpose.
Instead of reading every line straight through, start by reading the last one or two sentences to understand what the question is asking. Then go back and review the full scenario for context. This helps you zero in on what’s actually being tested.
3. Focus on key clues.
Identify the relevant positives and negatives in the patient’s history, labs, and exam. These details often point you toward the right answer and help you eliminate wrong answer choices that contradict the information provided.
4. Think like a clinician.
Step 2 questions usually center on patient care. Ask yourself: What would stabilize or help this patient first? Prioritize answers that reflect practical, real-world management you’ve seen on rotations.
5. Save the tricky ones for later.
Flag questions that stump you and come back to them later after finishing the rest of the block. This keeps your momentum going and prevents you from wasting valuable time. While Step 2 is different from Step 1 because every point counts, panicking won’t help.
Final Thoughts
Preparing for Step 2 CK can feel overwhelming. But building a structured study plan, approaching questions systematically, understanding question types, and practicing clinical reasoning makes it far more manageable. Remember, you’ve seen most of these clinical encounters during clerkships and shelf exams, you just have to apply all that knowledge you’ve gathered.
Now empowered with these tips and tricks, you can tackle Step 2 with confidence! Good luck with your studying and be sure to reach out to Blueprint tutors if you need any assistance.
For more (free!) tips from Blueprint tutors, check out these other posts:





