DO vs. MD: Two Pathways to One National Resident Matching Program (NRMP) in 2022 and Beyond
- by
- Feb 11, 2022
- Reviewed by: Amy Rontal, MD
Given the recent merger of osteopathic and allopathic accreditation and residency training,this blog post will help you understand the main similarities and differences between the current osteopathic and allopathic pathways at medical schools. We also correct some of the most common misconceptions about osteopathic physicians and the training they receive.
The field of osteopathic medicine has grown rapidly in the 21st century. Although the United States has fewer than 200,000 practicing osteopathic physicians, as compared to more than 900,000 allopathic physicians, the number of osteopathic physicians increased by approximately 80% between 2010 and 2020. Currently, more than 25% of medical students are enrolled in osteopathic programs. Many prospective medical students are considering whether to apply to allopathic programs, osteopathic programs or both. The choice isn’t as stark as it might seem. Students who choose the allopathic route are guaranteed to collaborate with osteopathic physicians on clinical care at some point during their medical career. They are also likely to have former osteopathic students as co-residents during their internship and residency. Because of this, it is crucial for all aspiring students and current practitioners alike to accurately understand the similarities and differences between osteopathic and allopathic medical training.
Where did osteopathic medicine originate?
Osteopathic medicine began in the late 1800s, when physician Andrew Still developed a medical ideology that emphasized comprehensive care of the whole person, preventative and holistic medical treatments, and manual techniques to promote musculoskeletal wellness . Although osteopathic medicine has evolved over time, it continues to emphasize these key principles. Osteopathic medical students receive a D.O. degree once they finish their education at one of the 37 accredited osteopathic medical schools in the United States.
What are allopathic medical schools?
Osteopathic education, like allopathic education, includes physiology, pathophysiology, diagnoses, and medical treatments. On the other hand, allopathic medical training does not typically include education about osteopathic manipulative medicine. Allopathic medical students receive an M.D. degree once they finish their education at one of the more than 150 allopathic medical schools in the United States.
Here are some common myths about osteopathic and allopathic medical schools:
Myth #1: Osteopathic physicians must incorporate osteopathic manipulative medicine into their clinical work
Osteopathic manipulative medicine (OMM) involves more than thirty specific techniques, such as the facilitated oscillatory release technique (the use of manually applied vibrations), the myofascial release technique (the use of manual force until a release is palpated), and the thoracic lymphatic pump (the application of pressure on the anterior rib cage during exhalation).
Only some osteopathic physicians incorporate OMM techniques into their clinical practice. Osteopathic physicians enter a variety of residency training programs and then work in many different medical specialties. Some osteopathic physicians practice surgical subspecialties, such as otolaryngology or urology, which focus on particular regions of the body and therefore may not be compatible with many OMM techniques. Moreover, those working in fields such as internal medicine, family medicine, or pediatrics do not typically incorporate OMM into their clinical practices.
- Fact #1: Osteopathic medical students receive training in osteopathic manipulative medicine techniques during their medical education
Although osteopathic physicians do not necessarily have to incorporate OMM into their clinical work, it is, indeed, generally taught at osteopathic medical schools but not allopathic medical schools.
Myth #2: Osteopathic physicians practice a comprehensive approach to medicine and wellness, which allopathic physicians do not practice
As the American Association of Colleges of Osteopathic Medicine states, osteopathic physicians “work in partnership with patients to help them achieve a high level of wellness by focusing on health education, injury prevention, and disease prevention” (AACOM). Nevertheless, comprehensive wellness and preventative medicine are core components of primary care medicine, which both allopathic and osteopathic physicians can practice. Both MD and DO primary care physicians routinely inquire about patients’ mental wellness, screen patients for psychiatric conditions such as depression, provide routine vaccinations, and counsel patients on health maintenance behaviors, including proper nutrition, weight loss, and regular exercise.
- Fact #2: Osteopathic physicians traditionally complete a one-year internship that provides broad clinical training
Osteopathic physicians traditionally complete a one-year internship that provides interns with broad clinical experiences in the fields of family medicine, obstetrics-gynecology, internal medicine, pediatrics, and surgery, thereby fostering a comprehensive view of patients’ medical needs. By contrast, allopathic internships typically focus on one of those medical fields. Both broad and specifically-focused internships are becoming increasingly available to osteopathic students.
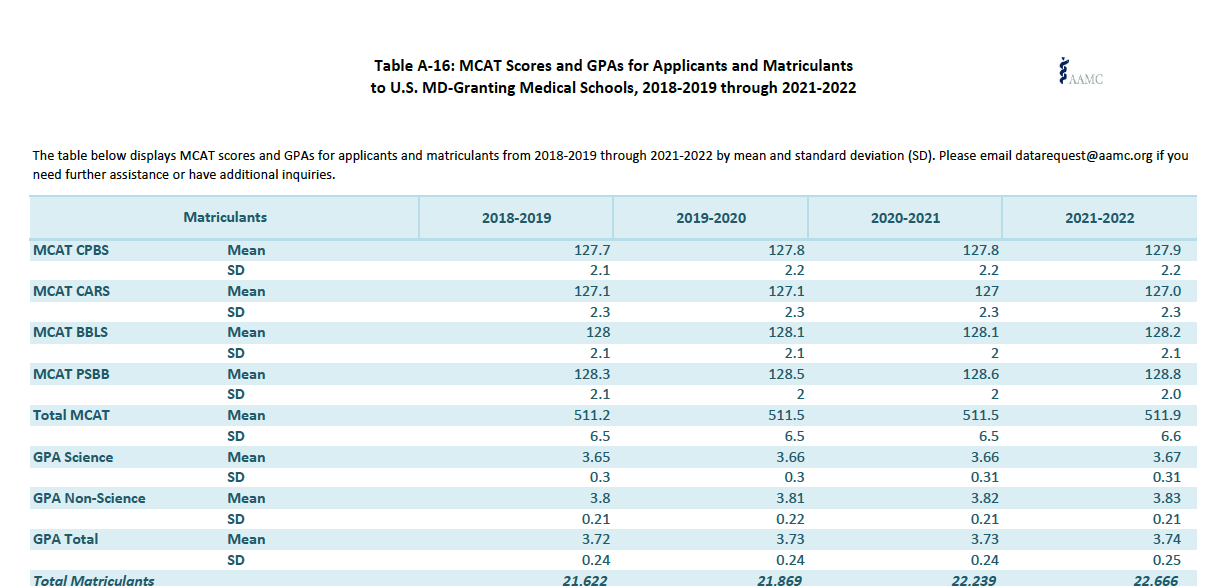
Myth #3: Osteopathic students had significantly lower GPAs or lower MCAT scores when they were applying to medical schools
Although the average MCAT scores and GPAs among enrolled students at osteopathic medical schools are typically lower than those of enrolled students at allopathic medical schools, these differences are merely statistical averages. For example, the average MCAT score of matriculated osteopathic students is 503.53, whereas the average MCAT score of matriculated allopathic students is 511.5, but the MCAT score ranges for matriculated osteopathic and allopathic students overlap. A variety of factors determine whether students matriculate into an osteopathic or allopathic medical school. tStudents’ objective data and performances on standardized exams form merely one component of their eventual career choices and decisions.
- Fact #3: Osteopathic and allopathic medical postgraduate training has combined into a single graduate medical education accreditation system
Although osteopathic students previously took the Comprehensive Osteopathic Medical Licensing Exam (COMLEX) series, whereas allopathic students took the United States Medical Licensing Exam (USMLE) series, osteopathic students can now take both sets of exams. Furthermore, osteopathic and allopathic students can currently apply to the same residency programs through the National Resident Matching Program (NRMP), which typically accepts either set of licensing exams.
Given this recent merger of allopathic and osteopathic residency education, medical school curricula remain the main distinction between allopathic and osteopathic training: osteopathic medical schools continue to put more emphasis than allopathic medical schools on integrated wellness and teach manipulative medicine techniques. Otherwise, the medical school curriculum for DO and MD is almost identical, and so are the premedical pathways. You should carefully consider the characteristics and focus of each type of medical school when deciding which option best fits you. None of these options is better or worse than the other one – it’s all about what suits you!