Aortic Dissection Management by Type for USMLE Step 1 & Step 2 CK
- by
- Jun 01, 2021
- Reviewed by: Amy Rontal, MD

In a recent webinar, a student asked, “Would it be important to know the management of aortic dissection depending on the type? Type A versus Type B, etc.” for USMLE Step 1 and/or USMLE Step 2 CK.
Drs. Michael Stephens and Sana Majid answer that question for you here—both in the video and the transcript below:
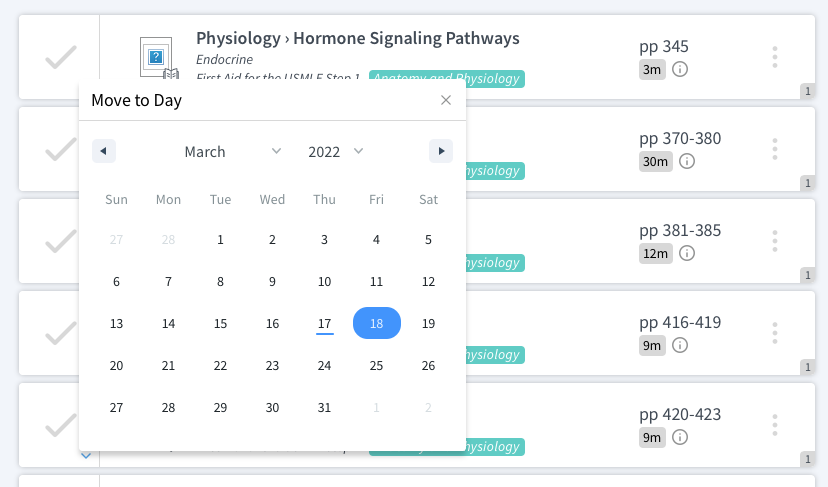
I think that there are different classification systems for aortic dissections. The one that I would home in on is the Stanford classification system where you have the Type A and Type B.
And I do think that it is relevant to understand the differences between them because—maybe not so much for Step 1, but very, very much so for Step 2 because it will inform your management of the aortic dissection going forward.
The Difference Between Type A and Type B Aortic Dissection:
Any time you have any component of an ailment of the ascending aorta, regardless of what’s going on with the rest of the aorta, you’re automatically Type A. I
f you have no involvement of the ascending aorta: you can have descending aorta involvement all the way down to the bifurcation, frankly. This is Type B.
So the way you differentiate is strictly on the basis of what’s going on with the ascending aorta.
The reason why we care: Type A dissection, especially, is a surgical emergency and there is a measurable increase in morbidity and mortality the longer you wait, the longer you delay surgical intervention. So think about surgery for a Type A dissection.
The difference, really, is with Type B. I don’t want to say absolutes, but often, perhaps most of the time, you would more medically manage a Type B dissection by bringing the patient’s blood pressure back under control, identifying and treating the underlying cause, which in the majority of the cases would be hypertension for whatever reason. That is the takeaway point in terms of thinking about management of aortic dissections. Sana, anything to add?
I think you nailed it. The big thing is the ascending aorta is where all the complications are that we were talking about, right? So, you can have a dissection into the subclavians, into the vertebrals, into the coronary arteries, that is life threatening complications versus lower down less so. So that’s really the distinction point.
The USMLEs are not going to have a very subtle distinction, but I think it is important to know when you’re going to do surgery, when surgery is indicated versus when it’s not. And of course, when the patient is unstable, then that’s a surefire way to say yes, go to surgery.
Want more micro-learning for med school and the USMLE, COMLEX, and Shelf exams? Check out our YouTube channel and social channels!