The first two years of medical school were wrought with references to things of which professors assumed we had innate knowledge. One that came up quite often was and receptors. For instance, when learning about pheochromocytoma, we were beat over the head with the dogma to “utilize blockade before administering a blocker.” Patient with a cocaine overdose? Tread lightly with blocker administration for fear of unopposed ‚-agonism! While we students could have parroted this information back with the greatest of ease, a proper foundation into what it all meant was lacking.
If you find yourself in said position, fret no longer. Knowledge of the adrenergic receptors, and their other G-protein cousins is essential to elevate your medical consciousness. We alluded to the absolute importance in our post on high-yield pharmacology for step 1, but this information is ultra-practical and can be applied to countless settings. Let us review, internalize, and grow more brilliant.
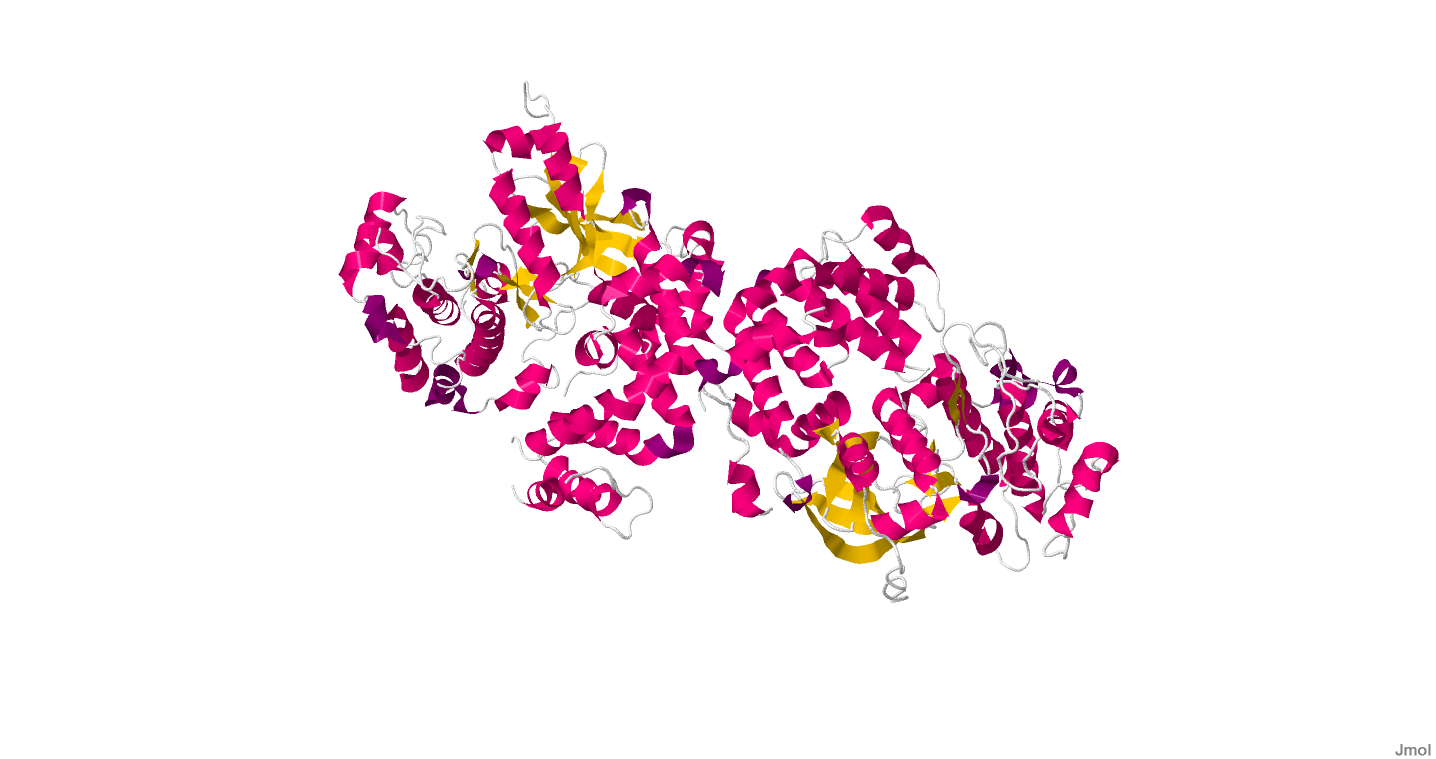
G-protein-coupled Receptors
A brief review of how G-protein-coupled receptors work: A G-protein is composed of a transmembrane receptor protein, with a heterotrimeric protein complement inside the cell. A molecule (e.g. epinephrine, acetylcholine) attaches to this receptor on the outside of the cell, causing dissociation of the trimeric protein inside the cell, signaling a cascade of second messengers inside the cell. When it comes to the autonomic nervous system, three types of G-proteins are relevant: Gs, Gi, and, like the popular men’s magazine, Gq. Gs proteins stimulate adenylyl cyclase, causing ATP to cyclo-fy into cAMP, which activates protein kinase A (PKA). Gi proteins have the opposite effect, inhibiting adenylyl cyclase, preventing the cascade from moving forward. Gq proteins utilize a different second messenger system involving inositol triphosphate (IP3) and diacylglycerol (DAG), leading to calcium influx and protein kinase C activation.
Now before you get basic scienced to death, let’s talk about clinical application. While many of these receptors are found in many different places en vivo, I’ll keep the discussion to the most clinically relevant sites.
1 Receptors
Located on vascular smooth muscle, activation (agonism) of these receptors causes contraction (vasoconstriction), and will increase blood pressure. Many of our vasopressors (epinephrine, norepinephrine, phenylephrine) have some degree of 1 agonism. These receptors are blocked (antagonized) by -zosin drugs (antihypertensive and BPH treatment), and phenoxybenzamine/phentolamine (pheochromocytoma medications).
2 Receptors
Far less important than 1. They utilize a Gi pathway, so agonism is inhibitory. They inhibit sympathetic outflow. Only two agonists here: clonidine and dexmedetomidine. Unsurprisingly, these drugs cause sedation and hypotension.
1 Receptors
Think HEART. Agonism of these Gs receptors causes increase PKA activity, leading to calcium influx. This in turn increases heart rate and contractility. Drugs that hit 1 receptors hard include epinephrine, dobutamine, and dopamine, hence their use in acute decompensated heart failure. Norepinephrine also has some ð›ƒ1 agonism, but is less potent than these other agents. These receptors are antagonized by blockers, which can decrease contractility and heart rate, and therefore, myocardial oxygen demand. Great for someone with coronary artery disease who is already suffering in terms of oxygen delivery to the myocardium.
2 Receptors
Biggest sites are smooth muscle of the vasculature supplying skeletal muscle & the uterus, and bronchioles. Agonism will relax the smooth muscle. This can happen around bronchioles causing bronchodilation (albuterol, salmeterol), in the uterus causing tocolysis (terbutaline), or in the skeletal muscles causing increased perfusion there. If you get lost, think what you administer to someone in bronchospasm (asthma attack). An emergency inhaled 2 agonist (albuterol), and if they are really suffering, epinephrine, which has 2 activity as well.
M1 Receptors
All muscarinic receptors are agonized by acetylcholine (ACh). Agonism here leads to increased salivation, increased gastric secretion, and bronchoconstriction. That’s why we use an antimuscarinic drug like ipratopium to open the bronchioles.
M2 Receptors
Like 1 receptors, THINK HEART. Unlike 1 receptors, agonism here decreases heart rate and contractility. Utilize an intravenous antimuscarinic like atropine to block these receptors, and cause an increase in heart rate. Recall that atropine is your first-line choice for symptomatic bradycardia.
Dopamine Receptors
Agonism of dopamine receptors can relax smooth muscle vasculature to the kidneys. These receptors are also widely distributed in the brain, and function in numerous pathways related to addiction, schizophrenia, and Parkinson’s disease. Parkinson’s disease is caused by lack of dopamine in the brain, so we treat it with a dopamine precursor (carbidopa-levodopa). Anti-dopaminergic drugs like metoclopramide and the antipsychotics can cause parkinsonism by blocking these receptors.
As a caveat, remember that while exogenous administration of dopamine will activate the dopamine receptor, it also activates and receptors in a dose dependent fashion, making it a useful choice in heart failure.
H1 Receptors
Histamine receptors are very important. H1 receptors are implicated in sinonasal and bronchial mucus production, as well as the endothelial permeability and bronchoconstrction seen in anaphylaxis. Activation of H1 receptors also causes itching. That’s why we administer antihistamines (e.g. diphenhydramine) for seasonal allergies, pruritus, and as an adjuvant to epinephrine for anaphylaxis.
H2 Receptors
H2 receptors are found in the stomach and stimulate gastric acid secretion. H2 blockers, like ranitidine, serve to decrease this acid production.
Vasopressin Receptors
Rounding out our G-protein receptors are the V1 and V2 receptors. The former are found along vascular smooth muscle. Agonism here causes vasoconstriction. That’s why vasopressin was once part of the ACLS ventricular fibrillation/tachycardia algorithm. Today, it is often used as a pressor in the ICU. V2 receptors are found in the distal tubules of nephrons. Their agonism leads to increased water reabsorption. Vasopressin’s other moniker, antidiuretic hormone, eloquently explains this action. Don’t pee! Reabsorb that water!
Hopefully this simple guide gives you a foundation in some of the body’s most important receptors. Now you can tell your from your understand how pressors function, and prevent studying from giving you an ulcer (hint: H2 blocker!).